| Research Article | ||
J Microbiol Infect Dis. 2023; 13(4): 190-195 J. Microbiol. Infect. Dis., (2023), Vol. 13(4): 190–195 Original Research A retrospective study on detection of herpesviruses in suspected herpes encephalitis patients in Sri LankaHewa Babarandage Chathurika Harshani, Denagama Vitharanage Rishan Geeth Ruwan, Jinadari Maduwanthi Munasinghe, Gamage Don Diluk Chathuranga and Janaki I Abeynayake*Medical Research Institute, Colombo, Sri Lanka *Corresponding Author: Janaki I Abeynayake. Medical Research Institute, Colombo, Sri Lanka. Email: janakiiabeynayake [at] yahoo.com Submitted: 24/09/2023 Accepted: 14/12/2023 Published: 31/12/2023 © 2023 Journal of Microbiology and Infectious Diseases
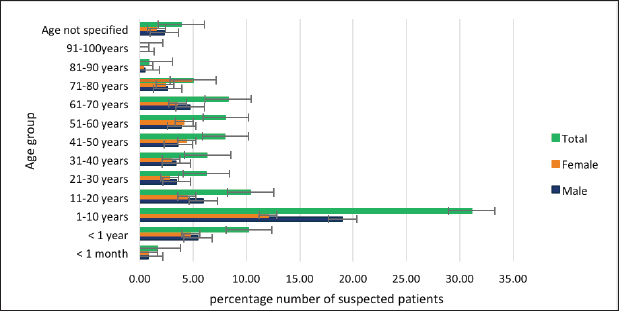
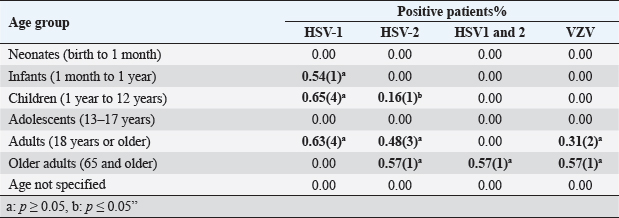
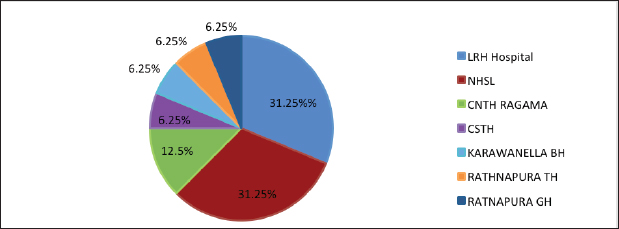
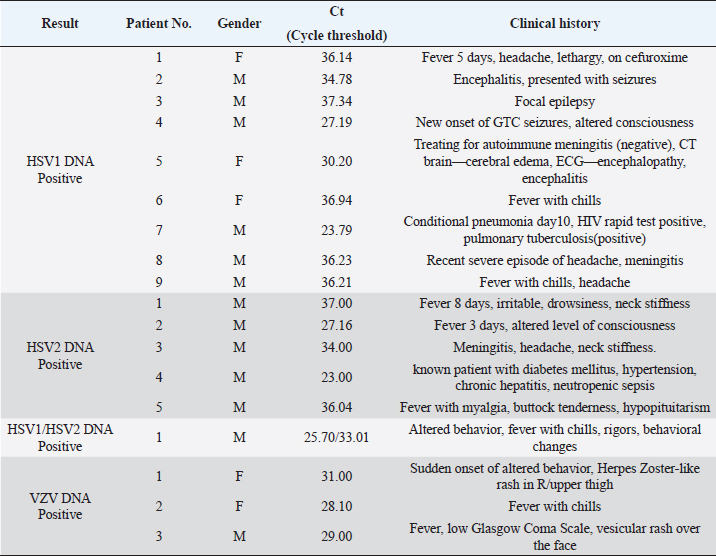
AbstractBackground: Encephalitis is a rare and serious brain infection that can be fatal. Viruses are common infectious agents causing encephalitis. Prompt detection of human herpes viruses in Cerebrospinal fluid (CSF) is crucial for early diagnosis and timely initiation of appropriate treatment, as this can significantly improve patient outcomes. Aim: This study aimed to determine the presence of herpes simplex virus (HSV) type 1, 2 (HSV-1, 2) and varicella–zoster virus (VZV) in CSF samples of suspected herpes encephalitis (HE) patients and to analyze demographic and associated clinical features. Method: All CSF samples from HE-suspected patients from different hospitals and/or facilities received at the Medical Research Institute in Sri Lanka from January 2022 to January 2023 were included in this retrospective study. Real-time polymerase chain reaction was used to detect HSV1, 2, and VZV in the samples. Results: From 1,801 suspected HE cases (mean age 25.67; range 2 days to 88 years; male: female; 1,003: 798), 18 (0.99%; male: female; 13: 5) were positive for herpes viruses; HSV-1(9, 0.50%), HSV-2 (5, 0.28%), HSV1 and 2 (1, 0.06%), and VZV (3, 0.17%). HSV-1 positivity: infants 0.54% (1/184), children 0.65% (4/618), and adults 0.63% (4/627). HSV-2: children 0.16% (1/618), adults 0.48% (3/627), and older adults 0.57% (1/175). VZV: adults 0.31% (2/627) and older adults 0.57% (1/175). Prominent symptoms: fever and headache. Conclusion: HSV-1, HSV-2, and VZV were detected in CSF samples as causative agents of encephalitis-suspected patients, and no significant association was observed with age groups. Further studies are needed for a proper conclusion. Keywords: Cerebrospinal fluid, Encephalitis, Herpes simplex virus, PCR, Varicella–zoster virus. IntroductionEncephalitis, characterized by inflammation of the cerebral parenchyma, manifests with neurological dysfunction and can result from immune system malfunctions or infections. Infectious agents such as viruses, bacteria, and fungi contribute to encephalitis, with human herpesviruses (HHV), particularly herpes simplex viruses (HSVs) and varicella–zoster virus (VZV), recognized as significant causative agents (Glaser et al., 2006). This study delves into the epidemiology of herpesvirus-related encephalitis, focusing on HSV-1, HSV-2, and VZV, with the aim of enhancing our understanding of the prevalence, clinical manifestations, and demographic patterns of these infections in suspected encephalitis patients in Sri Lanka. HSV, particularly HSV-1 and HSV-2, are known to trigger a broad spectrum of neurological manifestations (Bergström et al., 2021; Silva et al., 2022). Herpes simplex encephalitis (HSE) is a rare but severe manifestation of HSV infection, affecting approximately 1 in 250,000–500,000 people annually globally (Babaei et al., 2021). The clinical presentation of HSV encephalitis includes fever, headache, altered consciousness, focal neurological signs, and seizures (Whitley et al., 1986; Babaei et al., 2021). Mortality rates for untreated cases can reach 70%, and even with the administration of necessary therapy, a significant proportion of patients may experience persistent neurological abnormalities (Whitley and Baines, 2018). While HSV-1 is the predominant cause of HSE in adults and children, HSV-2 is associated with HSE in newborns with disseminated infection and immunocompromised individuals (Kennedy and Chaudhuri, 2002). VZV is another member of the herpesvirus family that can cause encephalitis. Particularly, it accounts for a significant portion of pediatric encephalitis cases in developed countries (Lohitharajah et al., 2017; Dheerasekara et al., 2020). The diversity in clinical manifestations and potential complications of herpesvirus infections necessitates thorough diagnostic approaches for timely and effective management. Cerebrospinal fluid (CSF) molecular testing for HSV infection, particularly using real-time polymerase chain reaction (PCR), has proven to be an extremely sensitive and specific approach (Basso et al., 2020). This method has replaced brain biopsy as the gold standard for diagnosing HSE and herpes meningitis (Schremser et al., 2020). Early detection of HSV-1 and HSV-2 in CSF using real-time PCR is critical for timely intervention, especially within the first week after symptom onset (DeBiasi et al., 2002). Delaying treatment or initiating acyclovir therapy after 3–5 days can significantly impact the sensitivity of PCR (DeBiasi et al., 2002). PCR for HSV-DNA and VZV-DNA is included in the first-line virology test panel for clinically suspected acute central nervous system infections in adult patients (Basso et al., 2020). This retrospective study aimed to provide a comprehensive overview of the detection of herpesviruses (HSV-1, HSV-2, and VZV) in CSF samples from encephalitis-suspected patients. The study spanned the period between January 2022 and March 2023, aiming to analyze real-time PCR results in conjunction with demographic and clinical characteristics. Materials and MethodsThis laboratory-based retrospective investigation involved the analysis of CSF samples received at the National Reference Virology Laboratory, Medical Research Institute, Sri Lanka, between January 2022 and March 2023. The age distribution of positive patients was categorized according to the age designations of the American Medical Association (NIH, 2023). DNA extraction from CSF samples utilized BioFlux, following the manufacturer’s recommended methodology. Real-time PCR assays were performed using commercial kits for HSV-1, HSV-2, and VZV (artus® HSV-1/2 RG PCR Kit, artus® VZV RG PCR Kit, QIAGEN GmbH, Germany). Demographic and clinical characteristics were extracted from request forms. In addition, previous records of HSV-positive patients were scrutinized for the presence of other encephalitis-causing agents, including enteroviruses, dengue, japanese encephalitis virus, adenoviruses, cytomegalovirus, influenza viruses, measles virus, rabies, and HIV, using real-time PCR or rapid test. Ethics approvals were waived for this study due to its retrospective nature and the absence of individual patients’ data reporting. Statistical analysisSPSS version 22.0 was employed for statistical analysis. Descriptive data, including mean, SD, and percentage, were analyzed using Microsoft Excel 2016 version. The chi-square test was utilized for examining categorical variables, considering a significance level of ≤0.05. ResultsOut of the 1,801 CSF samples collected from individuals with clinical suspicion of encephalitis, 55.7% were male, and 44.3% were female. The age distribution of suspected patients ranged from neonates to older adults, with the majority falling in the 1–10 years age group (Fig. 1). The samples were collected from 138 hospitals and/or facilities across various localities in Sri Lanka. HSV-1, HSV-2, HSV1&2, and VZV DNA were detected in 0.50%, 0.28%, 0.06%, and 0.17% of cases, respectively (Table 1). The majority of the positive cases were observed in adults, with a notable prevalence among males. Previous records of HSV-positive patients were examined for the presence of other potential encephalitis-causing agents. Previous real-time PCR records for HSV-positive patients showed no other encephalitis-causing viruses. However, one patient with recent pneumonia tested positive for HSV-1 on the 10th day, confirmed HIV positive for the rapid test, and had pulmonary tuberculosis. The majority of any tested herpes virus DNA-positive patient samples were found from Lady Ridgeway Hospital and the National Hospital of Sri Lanka (31.25%) (Fig. 2).
Fig. 1. The age and gender distribution of herpes suspected patients. Table 1. Categorization of encephalitis-positive patients with different age groups.
Fig. 2. The distribution of sample receiving centers of herpes virus-positive patients. Fever and headache emerged as the most common symptoms of herpes encephalitis (HE) across all tested herpes viruses. The study provided detailed insights into the clinical characteristics of positive cases, including Ct values, viral load, and specific manifestations in certain patients (Table 2). Among the patients who tested positive for HSV-1, HSV-2, and VZV, gender disparities were noted. HSV-2 positive cases were exclusively male, and HSV-1 positivity was more prevalent in males. The mean Ct values varied for different viruses, indicating potential differences in viral loads. DiscussionHHV infections, caused by HSV-1, HSV-2, and VZV, can lead to various skin and mucous membrane illnesses, including severe complications such as herpetic neuralgia and HE (Schremser et al., 2020). This retrospective study aimed to provide insights into the detection of HSV-1, HSV-2, and VZV in CSF samples from suspected encephalitis patients in Sri Lanka using real-time PCR over a 1-year period. The study also examined the demographic and clinical characteristics of suspected or positive HE patients. Several studies, including Dehghan et al. (2023), Fakhredini et al. (2023), and Ibrahim et al. (2005), have reported the occurrence of HSV and VZV in CSF samples of suspected HE patients. In contrast with Kleines et al. (2014), who found an association between age and positive viral PCR detection, our study, spanning 1,801 patients from 2 days to 88 years, did not detect such an association. Similarly, the prevalence rates of HSV-1 and HSV-2 in our study (9/1,801 and 5/1,801, respectively) were higher than those reported by Koskiniemi et al. (1997), highlighting the variability in herpesvirus prevalence across populations. In a study by Dehghan et al. (2023) involving 149 children, 7.3% showed viral DNA for herpes viruses. In our larger study (1,801 patients), HSV-1 and HSV-2 were detected in 0.65% and 0.16% of 618 children, respectively. This suggests a relatively lower prevalence among children in our population compared to the study done by Dehghan et al. (2023). Table 2. Categorization of clinical and demographic features of herpes virus-positive patients.
Examining a study by Babaei et al. (2021) on 200 CSF samples, which found 11.11% HSV-positive cases with a majority being older than 50, our study demonstrated a lower relative percentage of HSV detection (0.83%). This may imply regional variations in herpesvirus prevalence. Notably, VZV was associated with encephalitis in 0.17% of our suspected patients, emphasizing its role even in the absence of cutaneous manifestations. The observed disparity in viral etiologies, with HSV-1 being more prevalent in our study despite global reports favoring HSV-2 or VZV, may stem from environmental differences, cultural variances, or genetic susceptibility across populations. While Behzad-Behbahani et al. (2003) and Ziyaeyan et al. (2011) found no significant association between age, gender, and positive PCR results, our study deviates slightly. Although no substantial link was established between increasing age and positive results, a noteworthy connection emerged between HSV positivity and gender. Specifically, the gender distribution of HSV-positive cases was skewed toward males (15 males to 3 females), potentially influenced by our study’s male-heavy participant pool (1,003 males to 798 females). Despite strengths such as a substantial participant count from diverse sources across Sri Lanka, our study has limitations inherent to its retrospective nature. Some participants lacked data for CSF evaluations and clinical characteristics, limiting in-depth analysis. However, the study underscores the importance of herpesviruses as causative agents in CNS infectious diseases, necessitating further prospective research to delineate clinical characteristics and consequences of alpha herpes virus infections. ConclusionIn conclusion, this retrospective study sheds light on the detection of HSV-1, HSV-2, and VZV in CSF samples from suspected encephalitis patients in Sri Lanka. The findings emphasize the importance of real-time PCR in identifying causative agents in HE and contribute to our understanding of the clinical and demographic characteristics of herpesvirus infections. The study calls for further research with larger sample sizes to validate and expand upon these findings, providing a more comprehensive picture of herpesvirus-related encephalitis in the Sri Lankan context. AcknowledgmentThe authors express their gratitude to all the staff of the Department of Virology, Medical Research Institute, Sri Lanka. Conflict of interestThe authors declare that they have no competing interests. FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Authors contributionsStudy concept and design: JIA, HBCH; data analysis: HBCH, JIA, DVRGR, JMM, GDDC; Manuscript writing and reviewing: HBCH, JIA; Supervision: JIA. ReferencesBabaei, A., Shatizadeh Malekshahi, S., Pirbonyeh, N. and Moattari, A. 2021. Prevalence and clinical manifestations of herpes simplex virus infection among suspected patients of herpes simplex encephalitis in Shiraz, Iran. Virusdisease 32(2), 266–271; doi:10.1007/s13337-021-00680-9 Basso, L., Bönke, L., Aust, S., Gärtner, M., Heuser-Collier, I., Otte, C., Wingenfeld, K., Bajbouj, M. and Grimm, S. 2020. Antidepressant and neurocognitive effects of serial ketamine administration versus ECT in depressed patients. J. Psychiatr. Res. 123, 1–8; doi: 10.1016/j.jpsychires.2020.01.002 Behzad-Behbahani, A., Abdolvahab, A., Gholamali, Y.P., Roshanak, B. and Mahmood, R. 2023. Clinical signs as a guide for performing HSV-PCR in correct diagnosis of herpes simplex virus encephalitis. Neurol. India. 51(3), 341. Available via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6383335/ (Accessed 10 July 2023) Bergström, P., Trybala, E., Eriksson, C.E., Johansson, M., Satir, T.M., Widéhn, S., Fruhwürth, S., Michno, W., Nazir, F.H., Hanrieder, J., Paludan, S.R., Agholme, L., Zetterberg, H. and Bergström, T. 2021. Herpes simplex virus 1 and 2 infections during differentiation of human cortical neurons. Viruses 13(10), 2072; doi:10.3390/v13102072 DeBiasi, R.L., Kleinschmidt-DeMasters, B., Weinberg, A. and Tyler, K.L. 2002. Use of PCR for the diagnosis of herpesvirus infections of the central nervous system. J. Clin. Virol. 25, 5–11; doi:10.1016/s1386-6532(02)00028-8 Dehghan, G., Goudarzi, H., Saket, S., Kazemi Aghdam, M., Golrokh Mofrad, M. and Faghihloo, E. 2023. Detection of HSV-1, HSV-2 and VZV isolated from cerebrospinal fluid samples of children suspected to encephalitis. Adv. Biomed. Res. 12, 141; doi:10.4103/abr.abr_322_22 Dheerasekara, W., Attanayake, W., Raziya, M., Jayawardhana, B., Rajamanthri, R. and Muthugala, M. 2020. Alpha herpes virus infections in a group of patients clinically suspected of central nervous system infections in Sri Lanka: a brief laboratory report. Sri. Lankan. J. Infect. Dis. 10(1), 72–75; doi:10.4038/sljid.v10i1.8277 Fakhredini, K., Soleimanjahi, H. and Bamdad, T. 2023. Prevalence of herpes simplex viruses types 1 and 2 infections among suspected children of encephalitis in Kermanshah, Iran. Iran. J. Microbiol. 15(1), 149–154; doi:10.18502/ijm.v15i1.11931 Ibrahim, A.I., Obeid, M.T., Jouma, M.J., Roemer, K., Mueller-Lantzsch, N. and Gärtner, B.C. 2005. Prevalence of herpes simplex virus (types 1 and 2), varicella-zoster virus, cytomegalovirus, and human herpesvirus 6 and 7 DNA in cerebrospinal fluid of Middle Eastern patients with encephalitis. J. Clin. Microbiol. 43(8), 4172–4174; doi:10.1128/JCM.43.8.4172-4174.2005 Glaser, C.A., Honarmand, S., Anderson, L.J., Schnurr, D.P., Forghani, B., Cossen, C.K., Schuster, F.L., Christie, L.J. and Tureen, J.H. 2006. Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin. Infect. Dis. 43(12), 1565–1577; doi:10.1086/509330 Kennedy, P.G.E. and Chaudhuri, A. 2002. Herpes simplex encephalitis. J. Neurol. Neurosurg. Psychiatry. 73, 237–238. Kleines, M., Scheithauer, S., Schiefer, J. and Häusler, M. 2014. Clinical application of viral cerebrospinal fluid PCR testing for diagnosis of central nervous system disorders: a retrospective 11-year experience. Diagn. Microbiol. Infect. Dis. 80(3), 207–215; doi: 10.1016/j.diagmicrobio.2014.07.010 Koskiniemi, M., Korppi, M., Mustonen, K., Rantala, H., Muttilainen, M., Herrgård, E., Ukkonen, P. and Vaheri, A. 1997. Epidemiology of encephalitis in children. A prospective multicentre study. Eur. J. Pediatr. 156(7), 541–545; doi:10.1007/s004310050658 Lohitharajah, J., Malavige, N., Arambepola, C., Wanigasinghe, J., Gamage, R., Gunaratne, P., Ratnayake, P. and Chang, T. 2017. Viral aetiologies of acute encephalitis in a hospital-based South Asian population. BMC. Infect. Dis. 17(1), 303; doi:10.1186/s12879-017-2403-z NIH. 2023. Style guide. NIH. Bethesda, Maryland, USA. Available via: https://www.nih.gov/nih-style-guide/age (Accessed on 2023 July10) Schremser, V., Antoniewicz, L., Tschachler, E. and Geusau, A. 2020. Polymerase chain reaction for the diagnosis of herpesvirus infections in dermatology: analysis of clinical data. Wien. Klin. Wochenschr. 132(1–2), 35–41; doi:10.1007/s00508-019-01585-w Silva, S., Ayoub, H.H., Johnston, C., Atun, R. and Abu-Raddad, L.J. 2022. Estimated economic burden of genital herpes and HIV attributable to herpes simplex virus type 2 infections in 90 low- and middle-income countries: a modeling study. PLoS. Med. 19(12), e1003938; doi:10.1371/journal.pmed.1003938 Whitley, R.J., Alford, C.A., Hirsch, Martin, S., Schooley, R.T., Luby, J.P., Aoki, F.Y., Hanley, D., Nahmias, A.J. and Soong, S. 1986. Vidarabine versus acyclovir therapy in herpes simplex encephalitis. N. Engl. J. Med. 314(3), 144–149; doi:10.1056/nejm198601163140303 Whitley, R. and Baines, J. 2018. Clinical management of herpes simplex virus infections: past, present, and future. F1000Research 7, F1000 Faculty Rev-1726; doi:10.12688/f1000research.16157.1 Ziyaeyan, M., Alborzi, A., Haghighi, A.B., Jamalidoust, M., Moeini, M. and Pourabbas, B. 2011. Diagnosis and quantitative detection of HSV DNA in samples from patients with suspected herpes simplex encephalitis. Braz. J. Infect. Dis. 15(3), 211–214; doi:10.1016/s1413-8670(11)70177-5 | ||
| How to Cite this Article |
| Pubmed Style Harshani HBC, Ruwan DVRG, Munasinghe JM, Chathuranga GDD, Abeynayake JI. A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. J Microbiol Infect Dis. 2023; 13(4): 190-195. doi:10.5455/JMID.2023.v13.i4.4 Web Style Harshani HBC, Ruwan DVRG, Munasinghe JM, Chathuranga GDD, Abeynayake JI. A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. https://www.jmidonline.org/?mno=170598 [Access: January 25, 2026]. doi:10.5455/JMID.2023.v13.i4.4 AMA (American Medical Association) Style Harshani HBC, Ruwan DVRG, Munasinghe JM, Chathuranga GDD, Abeynayake JI. A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. J Microbiol Infect Dis. 2023; 13(4): 190-195. doi:10.5455/JMID.2023.v13.i4.4 Vancouver/ICMJE Style Harshani HBC, Ruwan DVRG, Munasinghe JM, Chathuranga GDD, Abeynayake JI. A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. J Microbiol Infect Dis. (2023), [cited January 25, 2026]; 13(4): 190-195. doi:10.5455/JMID.2023.v13.i4.4 Harvard Style Harshani, H. B. C., Ruwan, . D. V. R. G., Munasinghe, . J. M., Chathuranga, . G. D. D. & Abeynayake, . J. I. (2023) A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. J Microbiol Infect Dis, 13 (4), 190-195. doi:10.5455/JMID.2023.v13.i4.4 Turabian Style Harshani, Hewa Babarandage Chathurika, Denagama Vitharanage Rishan Geeth Ruwan, Jinadari Maduwanthi Munasinghe, Gamage Don Diluk Chathuranga, and Janaki I Abeynayake. 2023. A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. Journal of Microbiology and Infectious Diseases, 13 (4), 190-195. doi:10.5455/JMID.2023.v13.i4.4 Chicago Style Harshani, Hewa Babarandage Chathurika, Denagama Vitharanage Rishan Geeth Ruwan, Jinadari Maduwanthi Munasinghe, Gamage Don Diluk Chathuranga, and Janaki I Abeynayake. "A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka." Journal of Microbiology and Infectious Diseases 13 (2023), 190-195. doi:10.5455/JMID.2023.v13.i4.4 MLA (The Modern Language Association) Style Harshani, Hewa Babarandage Chathurika, Denagama Vitharanage Rishan Geeth Ruwan, Jinadari Maduwanthi Munasinghe, Gamage Don Diluk Chathuranga, and Janaki I Abeynayake. "A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka." Journal of Microbiology and Infectious Diseases 13.4 (2023), 190-195. Print. doi:10.5455/JMID.2023.v13.i4.4 APA (American Psychological Association) Style Harshani, H. B. C., Ruwan, . D. V. R. G., Munasinghe, . J. M., Chathuranga, . G. D. D. & Abeynayake, . J. I. (2023) A Retrospective Study on Presence of Herpesviruses in Suspected Herpes Encephalitis Patients in Sri Lanka. Journal of Microbiology and Infectious Diseases, 13 (4), 190-195. doi:10.5455/JMID.2023.v13.i4.4 |