| Review Article Online Published: 27 Dec 2024 | ||
J Microbiol Infect Dis. 2024; 14(4): 165-169 J. Microbiol. Infect. Dis., (2024), Vol. 14(4): 165–169 Review Article Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A reviewNaseem Fatima1, Syed Tasleem Raza1*, Vijay Kumar2 and Saliha Rizvi31Department of Biochemistry, Era’s Lucknow Medical College and Hospital, Lucknow, 226003, India 2Department of Surgical Oncology, King George’s Medical University, Lucknow, 226003, India 3Department of Biotechnology, Era University, Lucknow, 226003, India *Corresponding Author: Syed Tasleem Raza. Department of Biochemistry, Era’s Lucknow Medical College and Hospital, Lucknow, 226003, India. Email: tasleem24 [at] gmail.com Submitted: 10/09/2024 Accepted: 18/11/2024 Published: 31/12/2024 © 2024 Journal of Microbiology and Infectious Diseases
ABSTRACTHelicobacter pylori (H. pylori), is a bacterium with spiral-shaped Gram-negative characteristics, affects approximately 60% of the people in India. H. pylori infection is considered as one of the causes of gastric inflammation, which results in several gastric disorders such as the occurrence of ulcers in esophagus, stomach, and small intestine, which may further lead to gastric cancer. In addition, infection with H. pylori has also shows a positive association with gallbladder diseases including cholelithiasis, cholecystitis, gallbladder polyps, and gallbladder cancer. However, due to a lack of literature, the interconnection between H. pylori and gallbladder pathologies remains unknown. In this review, it was aim to provide an up-to-date summary of the link between the environment created by H. pylori and the development of gallbladder diseases. It was concluded that infection with H. pylori was linked to cholelithiasis, chronic cholecystitis, and gallbladder cancer. But available literature reports showed contradictory results. Therefore, a panel of in-depth studies is needed to establish the link between H. pylori-associated gallbladder diseases. Keywords: Helicobacter pylori, Cholecystitis, Cholelithiasis, Carcinoma, Gallbladder. INTRODUCTIONGallbladder disease (GB disease) is a common digestive system disorder affecting approximately 20% of healthy individuals worldwide. It often presents as cholecystitis, gallstones, and GB cancer. While the exact cause and pathophysiology of gallstones are still unknown, persistent infection is now recognized as a possible risk factor. In addition to lifestyle variables including heavy alcohol intake, hyperlipidemia, fatty liver, gender, family history, and ethnicity, gallstone development may be linked to a complex combination of genetic and environmental factors. Additionally, there is evidence to suggest that GB problems are significantly associated with internal conditions such as hepatitis C virus (HCV) infection, GB polyps, and numerous liver abnormalities. Furthermore, the existence of gallstones is assumed to be significantly influenced by the gastroduodenal environment, and Helicobacter pylori (H. pylori) is regarded to be a mediating factor for both gastric and extragastric illness. A persistent H.pylori infection may attach the bile duct and GB,among other organs. Helicobacter pylori belongs to a category of bacteria with microaerophillic and Gram-negative property. The discovery of this bacterium and its contribution in the development of gastric and peptic ulcer disease was reported by Warren and Marshall (Marshall 2002). Helicobacter pylori was described as a commonest type of bacteria present in almost 50% of the total world population, and classified as cancer-causing (group I carcinogen) by the International Agency for Research on Cancer (IARC 1994). It is now recognized as the main and specific infection cause of stomach cancer in the world, especially in the Chinese population. It is found to be associated with pathogenesis of human GB diseases, including GB inflammatory disease, and gallstones. and also found its strong linked to chronic gastric diseases, including all types of gastric cancer (Zhou et al. 2013; Zhang et al. 2015; Zhang et al. 2020; Wang et al. 2021; Kucuk et al. 2021). METHODOLOGYEpidemiology (H. pylori)The H. pylori infection found around the world, high infection rate was observed in low- or middle-income countries than in developed countries. Its infection shows continuous changing over the past decade. This changing is due to a decline in the prevalence of gastric disorders, including gastric carcinoma (Fuccio et al. 2010). The prevalence of H. pylori is dropping worldwide, according to this meta-analysis, especially between 2011 and 2022 (Li et al. 2023). Its prevalence found higher in southern and eastern countries of Europe, when compared with northern countries. High incidence of H. pylori infection is reported in China, suggest common cause of gastric cancer in the Chinese population (Zhu et al. 2014). Another cross-sectional study based on the presence of H. pylori infection showed a significantly increased rate of gastric disorders in urban areas when compared with rural areas (Makkar et al. 2020). In India, positive infection of H. pylori is found in 60% of the population, a high prevalence was reported in rural areas, causes gastric inflammation, which results in duodenal ulcer, peptic ulcer, and gastric ulcer diseases. Gastritis is one of the reasons for duodenal ulcer diseases, as well as the precursor lesion developed because of pangastritis found its association with gastric cancer. In recent years, the positivity of H. pylori has been reported in gallstone disease (Mahmood et al. 2020). Pathogenesis (H. pylori)Helicobacter pylori, after enters in the stomach of the host cell, established a certain conditions like, survive in acidic environment, attachment to the host cell with the help of bacterial adhesins/receptors interaction, and tissue damaging due to toxins released, which results in successful colonies formation, persistant infection, and disease pathogenesis (Kao et al. 2016). Four steps for H. pylori colonization and pathogenesis
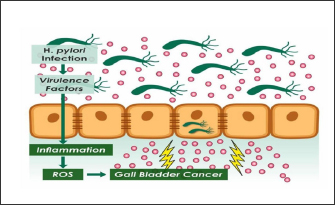
Figure 1. Schematic diagram of H. pylori infection and pathogenesis in the occurrence of gallbladder cancer. Relationship between H. pylori and GB diseasesHelicobacter pylori is a pathogenic bacterium found in the gastric mucous membrane that causes a variety of gastrointestinal disorders. Although research has been done to determine the relationship between bacterial virulence factors and the sort of inflammatory response that develops, however its regulatory mechanism that induces immune response and severity of inflammation is still not clear. GB inflammatory diseases and GB stone diseasesCholelithiasis and cholecystitis have been linked to H. pylori infection, albeit this association is less well-known. Many researchers have demonstrated that the potential cause of the GB diseases is the positivity of H. pylori in the gastrointestinal region. Additionally, numerous meta-analyses have studied into the connection between H. pylori infection associated with cholelithiasis and revealed that the presence of H. pylori DNA in the stomach of patients showed a significantly stronger risk for the development of gallstones than the patients with no H. pylori DNA. In a study , incidentally found H. pylori DNA in a GB mucosal lining of an individual detected with inflammation in GB tissue (Fatemi et al. 2018). Another study showed the presence of H. pylori in nearly 45% of the patients’ GB epithelium with gallstones (Kerawala et al. 2019). Similarly, a study found H. pylori DNA in the inflammated tissue of GB using RT-PCR, but no clinical correlation was found (Mishra et al. 2011). Gallstone prevalence was found to be significantly lower in H. pylori-eradicated patients (9.02% vs. 9.47%; p < 0.0001) compared to H. pylori-positive patients with no prior eradication. Furthermore, several other studies were also performed that demonstrated and confirmed the H. pylori infection, gallstones, GB inflammation, and bile in the GB (Mishra et al. 2013). Another study performed supported the interconnection between H. pylori and hepatobiliary stone disease (Xu et al. 2018). Several studies on the existence of H. pylori in GB have been performed and demonstrated a strong connection between H. pylori presence in GB (Dar et al. 2016). A meta-analysis on eighteen studies has been done, including 1061 patients with chronic cholecystitis/cholelithiasis. All the eighteen studies support the significant correlation between presence of H. pylori DNA and elevated risk of cholecystitis/cholelithiasis (Hassan et al. 2015). Conclusion drawn from the available literature on meta-analyses studies states that existence of H. pylori and gallstone disease shows decreased gallstone prevalence in patients who had previously had H. pylori removed. There are three major ways in which H. pylori infection can contribute to gallstone pathogenesis. At first, H. pylori might serve as a nidus for the formation of stone, providing a foundation for stone accumulation. Secondly, oxidative stress is elevated in the GB’s infected areas due to H. pylori infection. Bile supersaturation can occur as a result of the generation of reactive species of oxygen and nitrogen, which impacts the GB’s ability to absorb and secrete fluids and cause stones to form. Finally, H. pylori produces urease, it can enhance the precipitation of calcium bilirubinate. This enzyme stimulates the production of bile deconjugating enzymes and raises the pH for calcium precipitation (Cen et al. 2017; Hooi et al. 2017; Lem et al. 2023). However, the inability to demonstrate active H. pylori colonization of the GB limits these theories. GB polypsPresently, there are no authentic studies that suggest the interlinked connection between H. pylori and the occurrence of GB polyps. This may be because GB polyps are benign and fail to draw attention to potential risk factors. There have been contradictory findings from two prospective studies that studied the connection between GB polyps and positivity of H. pylori (Grigor’eva et al. 2020; Zhang et al. 2020). In a research involving 17,971 participants, found a positive statistically significant correlation between patients with GB polyps along with the infection of H. pylori. GB polyps were substantially more common in H. pylori-infected patients when compared with non-H. pylori-infected individuals (odd ratio=1.160, p=0.033). Thus, this study brought attention to the feasible association between positive H. pylori DNA and a localized inflammatory response, which could lead to a higher incidence of GB polyps (Kim et al. 2021). In contrast, another study was conducted which included 5,107 participants, did not find a significant correlation (p=0.110) between H. pylori infection and GB polyps (Grigor’eva et al. 2020). Due to the contradictory findings of the two studies, it is impossible to conclude about the possible interconnection between the occurrences of GB polyps because of the infection of H. pylori. Additional research, particularly prospective studies, is necessary to determine whether GB polyps and the presence of H. pylori DNA are causally related and, consequently, whether eradicating H. pylori can assists in the prevention of GB polyps. GB cancerThe bridge between the infection of H. pylori in an individual and GBC was a topic of research since past 10 years. This is because of insufficient evidence that provides the route by which H. pylori settles in the GB. Furthermore, several studies provided authentic evidences showing important and significant role of H. pylori in GBC. Study performed on tissue samples of GB diseases, found H. pylori positivity in 75% patients of GBC. Another study performed, which shows the positive culture of H. pylori in 44% of GBC patients (Kerawala et al. 2019). Research performed emphasized that GB metaplasia, adenomatous hyperplasia, and dysplasia changes were more frequently observed in an individual with positive to H. pylori infection (Xu et al. 2018). Research studies performed in the Indian population were concluded that northern area patients of benign GB disease also infected with H. pylori show higher prevalence when compared to the southern population (Mishra et al. 2011). Another study found H. pylori DNA in patients of cholecystitis and GBC (Dar et al. 2016). Using various bioinformatics predictors such as nuclear localization signal (NLS) mapper Balanced Subcellular Localization (BaCelLo) and HummPLoc 2.0, an insilico approach was used to investigate the targeting of H. pylori proteins into the nucleus of host cells. According to the findings of the study, several H. pylori proteins have been investigated as potential biomarkers for the early diagnosis, treatment, and cure of GBC (Zhou et al. 2013). By interfering with various pathways, including as transcription, translation, replication, and so on, these H. pylori nucleus-targeting proteins may change how host cells normally function. The regular growth and development of infected cells can be impacted by a variety of nucleus-targeting proteins. Our hypothesis is that H. pylori proteins that target host cell nuclei employ several mechanisms to control the expansion of gas bubble colonization. Numerous H. pylori proteins that may act as potential targets or biomarkers for early detection, treatment, or cure for gastric cancer were identified by these integrated bioinformatics studies (Wang et al. 2021). Though a large number of studies have been performed to study the interconnection between H. pylori and the occurrence of GBC, but all exiting studies unravel the environment created by H. pylori, which causes histopathological changes in the mucosal lining (hyperplasia, metaplasia, and lymphatic invasion) and further transformed to cancer. Therefore, further studies with exploration needed in this direction. CONCLUSIONH. pylori infection is associated with cholelithiasis, chronic cholecystitis, and gallbladder cancer in different ethnic groups globally.Since gallstones and H. pylori infections, both are prevalent condition across the world. It is critical to find out whether the removal of H. pylori will decrease the risk of GB diseases and thus may offer a novel approach to the management of such disease. However, available literature research reports showed contradictory results; therefore, longitudinal studies are required to establish the link between H. pylori and GB-related diseases. Thus, to fully comprehend the processes regulating this association and to assist elucidate the crucial aspect of illness prevention, more research is needed. ACKNOWLEDGMENTSNone. CONFLICT OF INTERESTThe authors declare that there is no conflict of interest. FUNDINGNone. REFERENCESCen, L., Pan, J., Zhou, B., Yu, C., Li, Y., Chen, W., and Shen, Z. 2017. “Helicobacter pylori infection of the gallbladder and the risk of chronic cholecystitis and cholelithiasis: a systematic review and meta-analysis.” Helicobacter 23(1), e-12457. Dar, M.Y., Ali, S., Raina, A.H., Raina, M.A., Shah, O.J., Shah, M.A., and Mudassar, S. 2016. Association of Helicobacter pylori with hepatobiliary stone disease, a prospective case control study. Indian J Gastroenterol 35(5), 343–346. Fatemi, S.M., Doosti, A., Shokri, D., Ghorbani-Dalini, S., Molazadeh, M., Tavakoli, H., et al. 2018. Is there a correlation between Helicobacter pylori and enterohepatic helicobacter species and gallstone cholecystitis? Middle East J Dig Dis 10(1), 24–30. Fuccio, L., Eusebi, L.H., and Bazzoli, F. 2010. Gastric cancer, Helicobacter pylori infection and other risk factors. World J Gastrointest Oncol 2(9), 342–347. Grigor’eva, I.N., and Romanova, T.I. 2020. Gallstone disease and microbiome. Microorganisms 8(6), 835. Hassan, E.H., Gerges, S.S., El-Atrebi, K.A., El-Bassyoun, H.T. 2015. The role of H. pylori infection in gall bladder cancer: clinicopathological study. Tumour Biol 36(9), 7093–7098. Hooi, J.K.Y., Lai, W.Y., Ng, W.K., Suen, M.M.Y., Underwood, F.E., Tanyingoh, D., et al. 2017. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology 153(2), 420–429. Howitt, M.R., Lee, J.Y., Lertsethtakarn, P., Vogelmann, R., Joubert, L.M., Ottemann, K.M., and Amieva M.R. 2011. ChePep controls Helicobacter pylori infection of the gastric glands and chemotaxis in the Epsilonproteobacteria. mBio 2(4), e00098–11. International Agency for Research on Cancer. 1994. Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Eval Carcinog Risk Hum 61(1), 177–241. Kao, C.Y., Sheu, B.S., and Wu, J.J. 2016. Helicobacter pylori infection: an overview of bacterial virulence factors and pathogenesis. Biomedi J 39(1), 14–23. Kerawala, A., Bakhtiar, N., Abidi, S., and Awan, S. 2019. Association of gallstone and Helicobacter pylori. J Med Sci 27(4), 269–272. Kim, K.H. 2021. Gallbladder polyps: evolving approach to the diagnosis and management. Yeungnam Univ J Med 38(1), 1–9. Kucuk, S., and Kucuk, I.G. 2021. The relationship between Helicobacter pylori and gallbladder pathologies, dysplasia and gallbladder cancer. Acta Med Mediterr 37(5), 2613–2620. Lertsethtakarn, P., Ottemann, K.M., and Hendrixson, D.R. 2011. Hendrixsonmotility and chemotaxis in Campylobacter and Helicobacter. Annu Rev Microbiol 65(3), 389–410. Li, Y., Choi, H., Leung K., Jiang F., Graham, D., and Leung, W. 2023. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 8(6), 553–564. Lim, K.P.K., Lee, A.J.L., Jiang, X., Teng, T.Z.J., and Shelat, V.G. 2023. The link between Helicobacter pylori infection and gallbladder and biliary tract diseases: a review. Ann Hepatobiliary Pancreat Surg 27(3), 241–250. Mahmood, A., Khan, Z., Razzaq, S., Mahmood, M.A., Ahmed, N., and Iqbal, W. 2020. The likelihood of Helicobacter pylori presence in pre cholecystectomy gall bladder with or without cholecystitis—a case control study. Pak J Med Health Sci 14, 304–306. Makkar, R., Butt, J., Huang, W.Y., McGlynn, K.A., Koshiol, J., Pawlita, M., et al. 2020. Seropositivity for Helicobacter pylori and hepatobiliary cancers in the PLCO study. Br J Cancer 123(6), 909–911. Marshall, B. 2002. Helicobacter pylori: 20 years on. Clin Med 2(2), 147–152. Matos, R., Amorim, I., Magalhaes, A., Haesebrouck, F., Gartner, F., and Reis, C.A. 2021. Adhesion of Helicobacter species to the human gastric mucosa: a deep look into glycans role. Front Mol Biosci 8, 656439. Mishra, R.R., Tewari, M., and Shukla, H.S. 2013. Association of Helicobacter pylori infection with inflammatory cytokine expression in patients with gallbladder cancer. Indian J Gastroenterol 32(4), 232–235. Mishra, R.R., Tewari M., and Shukla H.S. 2011. Helicobacter pylori and pathogenesis of gallbladder cancer. J Gastroenterol Hepatol 26(2), 260–266. Wang, Y., Imran, A., Shami, A., Chaudhary, A.A., and Khan, S. 2021. Decipher the Helicobacter pylori protein targeting in the nucleus of host cell and their implications in gallbladder cancer: an insilico approach. J Cancer 12(23), 7214–7222. Wang L, Chen J, Jiang W, Cen L, Pan J, Yu C, et al. 2021. The Relationship between Helicobacter pylori Infection of the Gallbladder and Chronic Cholecystitis and Cholelithiasis: A Systematic Review and Meta-Analysis. Can J Gastroenterol Hepatol. 6, 8886085. Xu, M.Y., Ma, J.H., Yuan, B.S., Yin, J., Liu, L., Lu, Q.B. 2018. Association between Helicobacter pylori infection and gallbladder diseases: a retrospective study. J Gastroenterol Hepatol 33(6), 1207–1212. Zhang FM, Yu CH, Chen HT, Shen Z, Hu FL, Yuan XP, et al. 2015. Helicobacter pylori infection is associated with gallstones: epidemiological survey in China. World J Gastroenterol 21(29), 8912–8919. Zhang, J., Zhang, Y., Chen, Y., Chen, W., Xu, H., and Sun, W. 2020. Helicobacter pylori is not a contributing factor in gallbladder polyps or gallstones: a case-control matching study of Chinese individuals. J Int Med Res 48(10), 300060520959220. Zhou, D., Guan, W.B., Wang, J.D., Zhang, Y., Gong, W., and Quan, Z.W. 2013. A comparative study of clinicopathological features between chronic cholecystitis patients with and without Helicobacter pylori infection in gallbladder mucosa. PLoS One 8(7), e70265. Zhu, Y., Zhou, X., Wu, J., Su J., and Zhang, G. 2014. Risk factors and prevalence of Helicobacter pylori infection in persistent high incidence area of gastric carcinoma in Yangzhong City. Gastroenterol Res Pract 2014, 481365. doi:10.1155/2014/481365. | ||
| How to Cite this Article |
| Pubmed Style Fatima N, Raza ST, Kumar V, Rizvi S. Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. J Microbiol Infect Dis. 2024; 14(4): 165-169. doi:10.5455/JMID.20240910060554 Web Style Fatima N, Raza ST, Kumar V, Rizvi S. Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. https://www.jmidonline.org/?mno=219675 [Access: January 07, 2026]. doi:10.5455/JMID.20240910060554 AMA (American Medical Association) Style Fatima N, Raza ST, Kumar V, Rizvi S. Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. J Microbiol Infect Dis. 2024; 14(4): 165-169. doi:10.5455/JMID.20240910060554 Vancouver/ICMJE Style Fatima N, Raza ST, Kumar V, Rizvi S. Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. J Microbiol Infect Dis. (2024), [cited January 07, 2026]; 14(4): 165-169. doi:10.5455/JMID.20240910060554 Harvard Style Fatima, N., Raza, . S. T., Kumar, . V. & Rizvi, . S. (2024) Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. J Microbiol Infect Dis, 14 (4), 165-169. doi:10.5455/JMID.20240910060554 Turabian Style Fatima, Naseem, Syed Tasleem Raza, Vijay Kumar, and Saliha Rizvi. 2024. Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. Journal of Microbiology and Infectious Diseases, 14 (4), 165-169. doi:10.5455/JMID.20240910060554 Chicago Style Fatima, Naseem, Syed Tasleem Raza, Vijay Kumar, and Saliha Rizvi. "Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review." Journal of Microbiology and Infectious Diseases 14 (2024), 165-169. doi:10.5455/JMID.20240910060554 MLA (The Modern Language Association) Style Fatima, Naseem, Syed Tasleem Raza, Vijay Kumar, and Saliha Rizvi. "Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review." Journal of Microbiology and Infectious Diseases 14.4 (2024), 165-169. Print. doi:10.5455/JMID.20240910060554 APA (American Psychological Association) Style Fatima, N., Raza, . S. T., Kumar, . V. & Rizvi, . S. (2024) Helicobacter pylori associated gallbladder diseases and their progression to gallbladder cancer: A review. Journal of Microbiology and Infectious Diseases, 14 (4), 165-169. doi:10.5455/JMID.20240910060554 |