| Research Article Online Published: 27 Dec 2024 | ||
J Microbiol Infect Dis. 2024; 14(4): 170-177 J. Microbiol. Infect. Dis., (2024), Vol. 14(4): 170–177 Research Article Hospital candidemia infection and related factors in intensive care unitsNurcan Çimen1* and Mehtap Sönmez21Adiyaman Eğitimve Araştırma Hastanesi, Kalp Damar Cerrahisi Kliniği, 02200, Turkey 2Kahramanmaraş Sütçü İmam Üniversitesi, Sağlık Bilimleri Fakültesi, Kahramanmaraş, 46100, Turkey *Corresponding Author: Nurcan Çimen. Adiyaman Eğitimve Araştırma Hastanesi, Kalp Damar Cerrahisi Kliniği, Turkey. Email: nkurt1992 [at] gmail.com Submitted: 25/07/2024 Accepted: 03/10/2024 Published: 31/12/2024 © 2024 Journal of Microbiology and Infectious Diseases
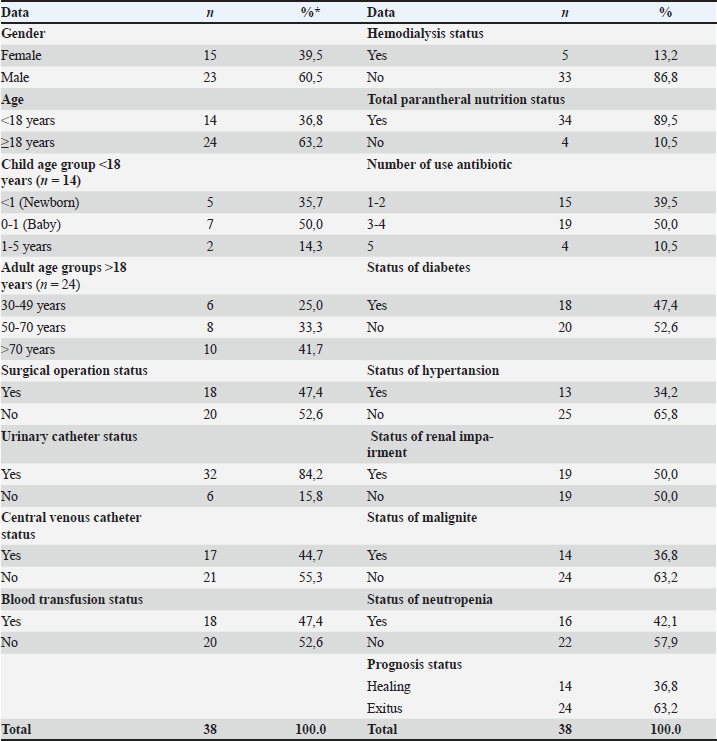
ABSTRACTBackground: Candida-related infections are the leading cause of healthcare-associated infections in intensive care units and are increasing day by day. Aim: This study was started in a university hospital in May 2018 and analyzed to determine candidemia, candiduria, and related factors seen in intensive care units between 2010 and 2015 years. Methods: A retrospective study included 38 patients who developed candidemia and were treated in intensive care for at least 72 hours. The data were presented as numbers and percentages and evaluated by the Chi-square test. Age, gender, history of surgical operation, presence of urinary catheter, presence of central venous catheter, history of blood transfusion, presence of hemodialysis, total parenteral nutritional status, diabetes, hypertension, renal failure, malig nancy, and neutropenia were compared according to candida type and candiduria. Results: The incidence of candida was 3.03% among the patients followed in the intensive care unit during the years included in the study, and the most common candida type was Candida albicans. Non-albicans Candida strains were more common in patients with renal insufficiency. It was determined that candiduria developed more in adult patients than in newborns. Patients with diabetes and malignancies were also found to develop more candiduria. Conclusion: Considering that candidemia causes high morbidity, prolongs hospital stay, and increases hospital costs, it can be seen that the importance of studies to determine the risk factors of candidemia has increased. Keywords: Intensive care, Candida, Candiduria, Associated factors. INTRODUCTIONHealthcare-associated infections, which are known as the most negative consequences of health care, are common all over the world and in Turkey. It has been reported that Healthcare Associated İnfection (HIA) affects 5%–20% of hospitalized patients in general, and in Europe, at least 7.5 million patients are exposed each year, and more than 147,000 people die directly or indirectly from this cause each year (Anderson 2019). Intensive care units are the most common hospital settings where infections are most common due to reasons such as immunosuppression of patients, prolonged hospitalization, long-term disability, antimicrobial resistance, and disease associated with socioeconomic conditions (Miyake et al. 2022; Jalaliet al. 2022). The European Center for Disease Prevention and Control (ECDC) reported in 2019 that 4% of all patients staying in intensive care units for more than 2 days developed pneumonia, 3% had bloodstream infections, and 2% developed urinary tract infections. The vast majority of these infections can be prevented by applying infection control methods. (ECDC 2016). Candida-related infections are the leading healthcare-associated infections in intensive care units. In studies on this, it has been reported that the average incidence of candidemia per 1000 patients in Europe, including 23 intensive care units, is 5.52. In another study, the prevalence of candidemia attacks per 1000 intensive care patients was reported as 6.87 (Basetii et al. 2019; Kett et al. 2011). Although Candida albicans is the cause of the majority of candidemia in intensive care units, it is observed that there is an increase in infections of non-albicans Candida. The increase in the frequency of use of antifungal drugs has increased the incidence of non-albicans Candida species. The most common species are Candida glabrata (C. glabrata), Candida guilliermondii (C. guilliermondii), Candida parapsilosis (C.parapsilosis), Candida krusei (C. krusei), Candida tropicalis (C.tropicalis), Candida lusitaniae (C.lusitaniae), and Candida zeylanoides (C. zeylanoides) (Altun et al. 2023). In some countries, C. glabrata is the most common, while in others, C. parapsilosis is seen. Although C. parapsilosis is a commensal microorganism of human skin, it can be transmitted from person to person through contaminated sources. In intensive care units, parenteral nutrition is becoming a worrisome species due to their location on inert substrates such as intravascular catheters (Töth et al. 2019; Martini et al. 2020; de Pauala et al. 2020). In a study involving 6 different centers in Turkey, 2,547 yeast isolates were obtained in a 6-year period. In intensive care units, C. albicans ranked first with 476 (45.2%) isolates, followed by C. parapsilosis complex (28.7%), C. glabrata (10.7%), and C .tropicalis (7.3%) (Ergon 2020). The most effective protection in Candidiasis is the maintenance of normal flora balance and an intact immune system. Although the main risk factors for the development of infection of candida species are factors that depress the immune system such as total parenteral nutrition status, presence of a central venous catheter, and use of broad-spectrum antibiotics, some researchers have expanded them to obtain different risk patient groups. In this study, it was conducted to determine the factors associated with candidemia of nosocomial infection. MATERIALS AND METHODSThis study is cross-sectional analytical. The data were collected retrospectively by examining the files of patients hospitalized in the intensive care unit of a university hospital between January 1, 2010 and December 31, 2015. A total of 1253 patients treated in intensive care units over a 5-year period were included in the study. Research inclusion criteria: “Candida spp. growth in blood culture” and “having been treated in the hospital for at least 72 hours.” While all candidemia patients between the ages of 1 and 92 years were included in the study, no exclusion criteria were determined. The diagnosis of candidemia and candiduria was made on the basis of CDC (Centers for Disease Control and Prevention) diagnostic criteria by creating sufficient colonies in the laboratory environment of the samples taken from the patients. The records of 1253 patients treated in the intensive care unit between January 1, 2010 and December 31, 2015 were examined, and 38 patients diagnosed with candidemia were included in the study based on the study inclusion criteria and CDC diagnostic criteria. All data included and diagnosed as candidemia were evaluated in accordance with the criteria of “identification of pathogenic microorganism by culture or non-culture microscopic tests in one or more blood samples taken for diagnosis and treatment, and the microorganism detected in the blood sample is not associated with infection elsewhere in the body.” There were no patients with episodes, and each patient was included in a one-time study and no reproductive sample was detected. It aims to evaluate the relationship between candidemia types (Candida types were typed by the automatic identification method (by a Phoenix device in microbiology laboratories), presence and prognosis of candiduria and demographic data, treatment process data, additional diagnosis, and symptom clinical conditions. This research questions: 1. Is there a relationship between the gender and age group of patients diagnosed with candidemia and the type of candidemia? 2. Is there a relationship between gender and age group of patients with candidemia and type of candidemia? 3. Is there a relationship between the presence of diabetes, hypertension, renal failure, malignancy, and neutropenia in patients with candidemia and the type of candidemia? Data collection toolsData collection form prepared according to the parameters determined by the researcher was created according to the demographic characteristics, treatment processes, additional diagnosis, symptoms, and clinical conditions of the patients, history information about the disease, drug use characteristics, and information about the detected candidemia. Data collection form: age, gender, disease history, presence of urinary catheter, presence of central venous catheter, history of blood transfusion, whether they received hemodialysis, total parenteral nutrition status, latest prognosis information, history of diabetes, history of hypertension, renal failure, malignancy, and neutropenia, type of underlying disease, if any, history of burns and trauma, antifungal and antibiotic use status, number and type of antibiotics used. It includes information about the type of candidemia detected, whether there is candiduria and prognosis. With this form, the hospital information system and patient files were scanned and data were collected. Dependent variables of the study: Type of candidemia, Diagnosis of candiduria, independent variables: gender, age, presence of catheter, history of blood transfusion, total parenteral nutrition, chronic disease, malignancy, neutropenia. Data analysisSPSS 22.0 package program was used for the evaluation and analysis of the data obtained from the research. Descriptive statistics were indicated in numbers and percentages. Mean and standard deviation were used for continuous data. Chi-square test was used to compare the categorical data obtained and to determine the relationship between the variables. The data were considered significant considering the margin of error of 0.05 at the 95% confidence interval (p < 0.05). Study limitationsThe study only included patients who were hospitalized in the intensive care unit for at least 72 hours at the university hospital between January 1, 2010 and December 31, 2015. RESULTSThe data of 38 patients diagnosed with candidemia were included in the study. Some data about these patients are presented in Table 1. The mean age of the patients was 42.66 ± 33.3 (Min: 1-Max: 92) years. It was found that 36.8% of the patients were under the age of 18 and were treated in the pediatric intensive care unit. It was determined that 63.2% of them were over the age of 18 and were treated in adult intensive care units. The mean number of days of hospitalization was 22.15 ± 16.91 (Min: 2-Max: 72). In the process of intensive care treatment of patients, It was determined that 47.4%of patients had a surgical operation,84.2% had a urinary catheter, 44.7% had a central venous catheter, 47.4% had blood transfusion during treatment, 13.2% had hemodialysis, and 89.5% received total parenteral nutrition. When the post-treatment prognosis was examined, it was found that 63.2% resulted in exitus; it was determined that 36.8% of them were discharged with healing.Although it is not statistically significant, it has been determined that most of exitus have additional diagnoses such as hypertension, diabetes, and neutropenia. Table 1. Distribution of some data of patients.
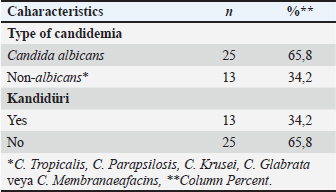
Table 2. Candidemia and candiduria characteristics.
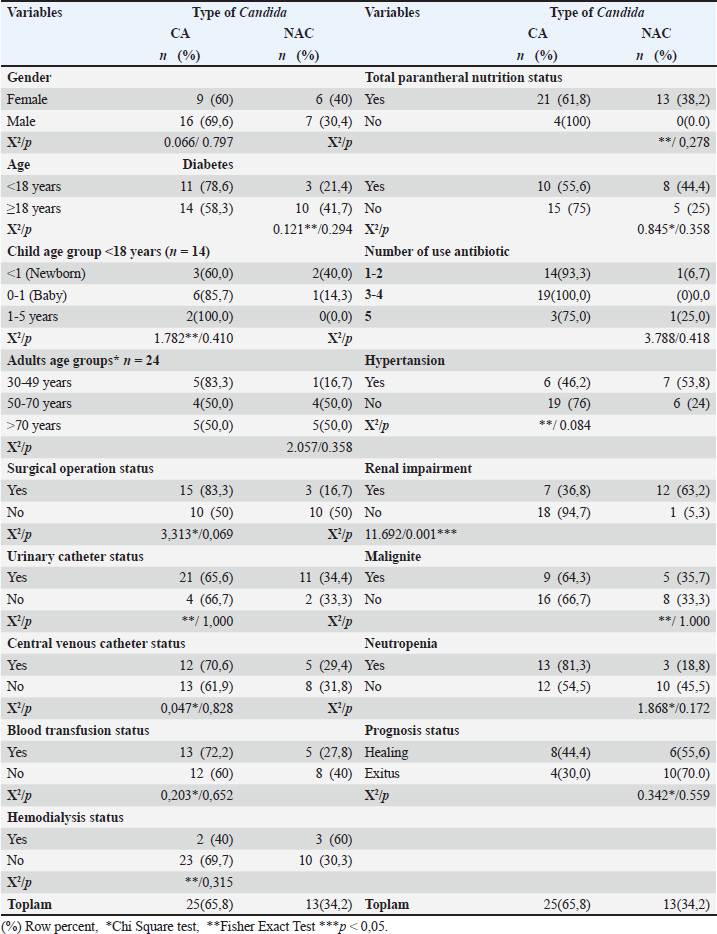
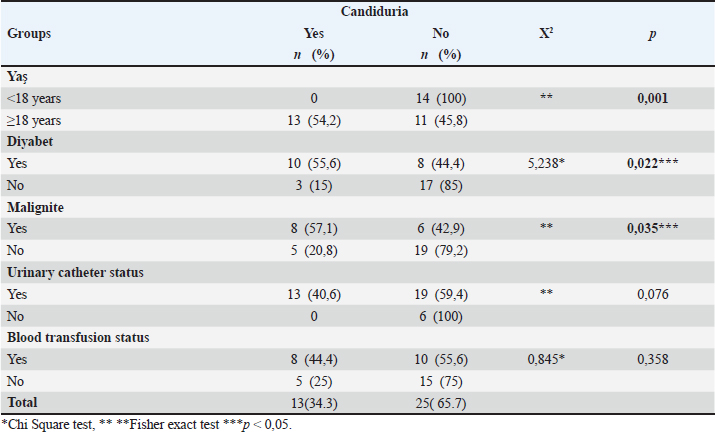
It was determined that 23.7% of the patients were admitted to the hospital due to gastrointestinal problems, 13.2% had cardiovascular, 13.2% had neurological diseases, and 13.2% had a history of infectious diseases. There were no patients with a history of burns or trauma as an indication for hospitalization. All of the patients received antibiotic therapy and antifungal therapy. Half of the patients used 3-4 different antibiotics. The antibiotics they use; it was observed that they used carbapenem the most, cephalosporin in second place, and penicillin in third place. Data on candidemia detected in patients are given in Table 2. When the types of candidemia detected in the patients included in the study were examined, C. albicans in 65.8%; non-albicans strains were found in 34.2% of them. It was determined that the detected non-albicans consisted of species such as C. tropicalis (n=5), C. parapsilosis (n=4), C. krusei (n=2), C. glabrata (n=1), and C. membranifaciens (n=1). In addition, candiduria was detected in 34.2% of the patients.Some data with candida species are compared in Table 3. The relationship between surgery, urinary catheter, central venous catheter, blood transfusion, hemodialysis, TPN, and Candida type was not statistically significant (p > 0.05). It was determined that more than half of the patients with candiduria underwent a urinary catheter and blood transfusion, although it was not statistically significant. The relationship between renal failure and candida type was found to be statistically significant (p < 0.05). Accordingly, it was observed that non-albicans Candida type was more common in patients with renal failure and C. albicans type was more common in patients without renal failure. The relationship between diabetes, hypertension, malignancy, neutropenia, and candida type was not statistically significant (p > 0.05). Some sociodemographic characteristics were compared with candiduria and given in Table 4. The relationship between age group and candiduria was found to be statistically significant (p < 0.05). Accordingly, it was observed that the development of candiduria was higher in adult patients than in newborns. It has also been determined that patients with diabetes and malignancy have more Candidia. DISCUSSIONCandida is one of the most important types of fungal infections that are becoming more common. It causes the rapid colonization of candida species on the human organism. Although invasive interventions such as catheter application to patients cause this colonization, it has been reported in the literature that the use of broad-spectrum antibiotics and abdominal surgery in patients hospitalized in intensive care units, those receiving immunosuppressive therapy, and abdominal surgery are factors that increase the risk of infection (Altun et al. 2023). In this study, 3. It was determined that there were 38 patients diagnosed with candida and candiduria in the intensive care units of a step-training and research hospital within a 5-year period. In a study, it was reported that 30 candidemia infections were produced in the one-year Intensive Care Unit, the majority of which were non-C. albicans species. In the same study, it was reported that the one-year incidence of candidemia was 14.72 per 1000 patients (Kerget et al. 2020). In a study conducted in a tertiary care hospital, 150 healthcare-associated (SHI) candidemias were detected in all clinics according to the patient files examined retrospectively between 2014 and 2019 (Çeviker et al. 2020). When the years covered by our study periods are compared with the years covered by other studies, it is seen that there is an increase in candida infections over the years. In this study, C. albicans was seen in 65.8%, while the incidence of other species was 34.2%. In the study conducted in a tertiary care hospital, it was reported that C. albicans was detected more than other species (66.3%), and C. albicans was the highest in all intensive care units where the study was conducted (Eren et al. 2023). Candida albicans has been frequently reported in Serbia, China, Australia, and Turkey. Candida albicans was reported to be most frequently isolated in Serbia (Arsic et al. 2018), China (Guo et al. 2017), Australia (Chapman et al. 2017), the Netherlands (Wouters et al. 2018), and Turkey (Yeşilkaya et al. 2007; Bilgi et al. 2015). It is seen that the majority of patients with candidemia are adults. In our study, it was determined that 63.2% were 18 years of age or older. Candida species were detected in 176 (11.2%) of a total of 1576 clinical urine samples in India, while the incidence rate was high in the 21–30 age group, it was reported that the lowest incidence was in the 71–80 age group (Mishra et al. 2022). In a study conducted in pediatrics clinics, it was reported that candida infection was detected in 37 cases over a period of 4 years (Ertek 2020). In another study, the mortality rate from candidemia was 9.5% in children (Çetin et al. 2024). In a study conducted in a tertiary care hospital, it was reported that the most frequently isolated species from all samples were C. albicans (n=185/279, 66.3%), while it was seen in the pediatric intensive care unit (n=11/17, 64.7%) (Eren et al. 2023) This shows that candida infections are more common in adult patients. Table 3. Comparison of some data with Candida species.
In this study, although there was no significant relationship between surgical operation, urinary catheter, central venous catheter, blood transfusion, hemodialysis, TPN, and Candida type, it was seen that the patients with the most Candida in accordance with the literature, underwent surgical operation, had a central catheter inserted, had blood transfusions, were fed with TPN, and were diagnosed with DM, malignancy, and neutropenia. Among the reasons that increase the likelihood of Candida infections in intensive care units, conditions that cause systematic deterioration of host defenses such as neutropenia, DM, malignancy, invasive procedures such as surgery, catheter insertion, TPN ILR nutrition, and localization in the gastrointestinal tract such as using broad-spectrum antibiotics have been reported (Holley et al. 2009; Paiava et al. 2016). In this study conducted in intensive care units, candiduria was not detected in pediatric intensive care units and was mostly seen in patients with DM and malignancy (p < 0.05). Many studies in the literature have reported diabetes mellitus, urinary tract defects, genitourinary tuberculosis, malignancy, chronic renal failure, neutropenia, immunosuppressive therapy, antimicrobial use, presence of foreign bodies in the urinary system, hemodialysis, surgical intervention, and kidney transplantation as risk factors for candiduria (Paul et al. 2004; Alpat et al. 2011; Montravers et al. 2016; Powers et al. 2016; Conway et al. 2015; Galiczewski and Shurpin 2016). Table 4. Comparison of candiduria and some sociodemographic characteristics.
The increase in nosocomial infections and antimicrobial resistance is a burden for healthcare. Considering that candidemia causes a high morbidity, prolongs hospital stay, and increases hospital costs, it can be seen that the importance of studies to determine the risk factors of candidemia has increased. Reducing the mortality rate of 30% to 60% for candidemia (Hirano et al. 2015) can be achieved by preventing risk factors. As a result, we encounter higher infection rates in healthcare-associated infections intensive care units. One of the causes of these infections, Candida spp., is the most common fungal species in intensive care units. C. albicans, which is frequently seen, is more common in adults. Surgical operation, urinary catheter, central venous catheter, blood transfusion, hemodialysis, and TPN are related factors that increase the incidence of candida. ACKNOWLEDGMENTSWe would like to thank our faculty members who served in the nosocomial infections committee for their support in the realization of this study. Ethical approvalBefore the research, approval was obtained from the Clinical Research Ethics Committee of Kahramanmaras Sutcu İmam University (21.03.2018/24). In addition, in order to access the data of the research, permission was obtained from the chief physician of Kahramanmaras Sutcu Imam University Health Practice and Research Hospital. Ethics Committee Approval and Application Permission are included in the appendix of the research. FundingNo Funding. Author ContributionsNK, MS: Conceptualization, Investigation, Resources, Data Curation, Writing—Review and Editing, Supervision. Conflict of InterestThere was no conflict of interest between authors. Data AvailabilityThis study was produced from the master’s thesis (2019/553365). The data can be accessed if requested from the corresponding author. REFERENCESAlpat, S.N., Özgüneş, İ., Ertem, O.T., Erben, N., Kartal, E.D., and Tozun, M. 2011. Kandidürisi Olan Hastalarda Risk Faktörlerinin Değerlendirilmesi. Mikrobiyol Bul 45(2), 318–324. Altun, G., Akbaş, T., and Yekenkurul, D. 2023. İnvazif Kandida Enfeksiyonu. SABD 13(1), 156–164. Andersen, B.M. 2019. Hospital infections: surveillance. In: Prevention and Control of Infections in Hospitals: Springer International Publshing, Norway, pp. 13–22 Arsic Arsenijevic, V.S., Otašević, S., Dragana, J., Minic, P., Matijasevic, J., Medić, D., et al. 2018. Candida bloodstream infections in Serbia: first multicentre report of a national prospective observational survey in intensive care units. Mycoses 61(2), 70–78. Bassetti, M., Giacobbe, D.R., Vena, A., Trucchi, C., Ansaldi, F., Antonelli, M., et al. 2019. Incidence and outcome of invasive candidiasis in intensive care units (ICUs) in Europe: results of the EUCANDICU Project. Crit Care 231, 219. Avaliable from: https://Doi. Org/10.1186/S13054-019-2497-3 Bilgi, E.A., Sav, H., Zararsız, G., Özakkaş, F., and Kiraz, N. 2015. Distribution of Candida species isolated from blood cultures in a university hospital. Dicle Medi J 3(42), 368–372. Çetin, F.T., Çay, Ü., Polat, M., Kılınç, F., Ünal, A., Tapaç, N.N., et al. 2024. Candida parapsilosis candidemia in children admitted to a tertiary hospital in Turkey: clinical features and antifungal susceptibility. Microbiol Spectr 12(7), e00564–24. doi: 10.1128/spectrum.00564-24. Epub 2024 Jun 12. PMID: 38864624; PMCID: PMC11218525. Çeviker, S.A., Günal, Ö.,Kılıç, S.S., Köksal, E., and Tahmaz, A. 2020. Üçüncü Basamak Hastanede Sağlık Hizmetiİle İlişkili Kandidemilerin Epidemiyolojisive Mikrobiyolojik Özellikleri: Tek Merkez Deneyimi. Muğla Sıtkı Koçman Üniversitesi Tıp Dergisi 7(1), 12–17. Chapman, B., Slavin, M., Marriott, D., Halliday, C., Kidd, S., Arthur, I., et al. 2017. Changing epidemiology of candidemia in Australia. J Antimicrob Chemother 72(4), 1103–1108. Conway, L.J., Carter, E.J., and Larson, E.L. 2015. Risk factors for nosocomial bacteremia secondary to urinary catheter-associated bacteriuria: a systematic review. Urol Nurs 35(4), 191–203. De Paula Menezes, R., De Oliveira Melo, S.G., Bessa, M.A.S., Silva, F.F., Alves, P.G.V., Araújo, L.B., et al. 2020. Candidemia by Candida parapsilosisin a neonatal intensive care unit: human and environmental reservoirs, virulence factors, and antifungal susceptibility. Braz J Microbiol 51(3), 851–860. doi:/10.1007/S42770- 020-00232-1. Eren, E., Sav, H., and Beştepe Dursun, Z. 2023. Araştırma hastanesinde yoğun bakım unitelerindeki hastalardan izole edilen Candida türlerinin epidemiyolojisi ve antifungal duyarlılığı. Türk Hijyen ve Deneysel Biyoloji Dergisi 79(1), 93–102. Ergon, M.C., Dereli, M.D., Atalay, M.A., Koç, A.N., Çerikçioğlu, N., Erturan, Z., and Aksaray, S. 2020. Türkiye’de Altı Yıllık Zaman Dilimiİçerisinde Kan Kültürlerinden Soyutlanan Maya Mantarlarının Tür Dağılımı: Çok Merkezli Bir Çalışma. Mikrobiyol Bul 54(4), 638–646. doi:10.5578/Mb.69837 Ertek, S. 2020. Bursa Uludağ Üniversitesi Tıp Fakültesi Çocuk sağlığı ve hastalıkları kliniklerinde kandidemi saptanan olgularda risk faktörlerinin belirlenmesi: beş yıllık retrospektif Çalışma. Uzmanlık Tezi, Bursa.https://tez.yok.gov.tr/UlusalTezMerkezi/tezDetay.jsp?id=UxrlmBbcPUbN253bwf4yyA&no=z2XitcyMHRJP8tHsbrNIAQ European Centre for Disease Prevention and Control. 2023. Annual Epidemiological Report For 2019 – Healthcare Associated İnfections Acquired İn İntensive Care Units. In: ECDC. Annual Epidemiological Report for 2018. Stockholm: ECDC. Galiczewski, J.M., Shurpin, K.M. 2016. An intervention to improve the catheter associated urinary tract infection rate in a medical intensive care unit: direct observation of catheter insertion procedure. Intensive Crit Care Nurs 32(40), 26–34. doi:10.1016/J. İccn.2016.12.003. Guo, L.N., Xiao, M., Cao, B., Qu, F., Zhan, Y.L, Hu, Y.J, et al, 2017. Epidemiology and antifungal susceptibilities of yeast isolates causing invasive infections across urban Beijing, China. Future Microbiol. 12:12,1075–1086. doi:10.2217/fmb-2017-0036. Hirano R, Sakamoto Y, Kudo K, Ohnishi M. 2015. Retrospective analysis of mortality and Candida isolates of 75 patients with candidemia: a single hospital experience. Infect Drug Resist 8;8:199–205. doi: 10.2147/IDR.S80677 Holley, A., Dulhunty, J., Blot, S., Lipman, J., Lobo, S., and Dancer, C. 2009. Temporal trends, risk factors and outcomes in albicans and non-albicans candidemia: an international epidemiological study in four multidisciplinary intensive care units. Int J Antimicrob 33(6), 554.e1–7. doi:10.1016/J.İjantimicag.2008.10.035 Jalali, Y., Sturdik, I., Jalali, M., Kyselovic, J., Liptakova, A., Kolosova, A., et al. 2022. First report of nosocomial outbreak of vancomycin-resistant Enterococcus faecium infection among COVID-19 patients hospitalized in a non-intensive care unit ward in Slovakia. Bratisl Lek Listy 123(8), 543–549. doi:10.4149/BLL_2022_086. Kerget, F., Karaşahin, Ö., Çelik, N., Kerget, B., and Yılmaz, S. İ. 2020. Yoğun Bakım Ünitesinde Hasta Örneklerinden İzole Edilen Kandida Türlerinin ve Kandidemi Risk Faktörlerinin Değerlendirilmesi. Bozok Tıp Dergisi 10(4), 55–61. Kett, D.H., Azoulay, E., Echeverria, P.M., Vincent, J.L., and Extended Prevalence of Infection in ICU Study (EPIC II) Group of Investigators. 2011. Candida bloodstream infections in intensive care units: analysis of the extended prevalence of infection in intensive care unit study. Crit Care Med 39(4), 665–670. Martini, C,. Torelli, R., De Groot, T., De Carolis, E., Morandotti, G.A., De Angelis, G., et al. 2020. Prevalence and clonal distribution of azole-resistant Candida parapsilosis isolates causing bloodstream infections in a large Italian hospital. Front Cell Infect Microbiol, 25:10, 232. doi:/10.3389/ Fcimb.2020.00232 Mishra, N., Kumari, D., and Mishra, A. 2022. Prevalence of Candida species in urinary tract infections from a tertiary care hospital at Lucknow, Uttar Pradesh, India: a retrospective study. Natl Lab Med 11(4), MO16–MO19. Miyake, A., Gotoh, K., Iwahashi, J., Togo, A., Horita, R., Miura, M., et al. 2022. Characteristics of biofilms formed by C. parapsilosis causing an outbreak in a neonatal intensive care unit. J Fungi 8(7), 700. doi:10.3390/Jof8070700. Montravers, P., Blot, S., Dimopoulos, G., Eckmann. C., Eggimann, P., Guirao, X, et al. 2016. Therapeutic management of peritonitis: a comprehensive guide for intensivists. Intensive Care Med 42(8), 1234–1247. Paiva, J.A., Pereira, J.M., Tabah, A., Mikstacki, A., De Carvalho, F.B., and Koulenti, D. 2016. Characteristics and risk factors for 28-day mortality of hospital acquired fungemias in ICVs: data from the EUROBACT Study. Crit Care 20(1), 53. Paul, N., Mathai, E., Abraham, O.C., and Mathai, D. 2004. Emerging microbiological trends in candiduria. Clin Infect Dis 39(11), 1743–1744. Powers, J. 2016. Impact of an aseptic procedure for breaking the integrity of the urinary drainage system on the development of catheter-associated urinary tract infections in the intensive care unit. Intensive Crit Care Nurs Dec2016:37, 82–85. Töth, R., Nosek, J., Mora-Montes, H.M., Gabaldon, T., Bliss, J.M., Nosanchuk, J.D., et al. 2019. Candida Parapsilosis: from Ggnes to the bedside. Clin Microbiol Rev 32(2), e00111–18. doi: 10.1128/Cmr.00111-18 Wouters, Y., Roosenboom, B., Causevic, E., Kievit, W., Groenewoud, H., and Wanten, G.J.A. 2018. Clinical outcomes of home parenteral nutrition patients using taurolidine as catheter lock: a long-term cohort study. Clin Nutr 38(5), 2210–2218, Yeşilkaya, A., Azap, Ö., Aydın, M., and Akçil Ok, M. 2017. Epidemiology, species distribution, clinical characteristics and mortality of candidemia in a tertiary care university hospital in Turkey, 2007–2014. Mycoses 60(7), 433–439. | ||
| How to Cite this Article |
| Pubmed Style Cimen N, Sonmez M. Hospital candidemia infection and related factors in intensıve care units. J Microbiol Infect Dis. 2024; 14(4): 170-177. doi:10.5455/JMID.20240823100803 Web Style Cimen N, Sonmez M. Hospital candidemia infection and related factors in intensıve care units. https://www.jmidonline.org/?mno=216883 [Access: January 25, 2026]. doi:10.5455/JMID.20240823100803 AMA (American Medical Association) Style Cimen N, Sonmez M. Hospital candidemia infection and related factors in intensıve care units. J Microbiol Infect Dis. 2024; 14(4): 170-177. doi:10.5455/JMID.20240823100803 Vancouver/ICMJE Style Cimen N, Sonmez M. Hospital candidemia infection and related factors in intensıve care units. J Microbiol Infect Dis. (2024), [cited January 25, 2026]; 14(4): 170-177. doi:10.5455/JMID.20240823100803 Harvard Style Cimen, N. & Sonmez, . M. (2024) Hospital candidemia infection and related factors in intensıve care units. J Microbiol Infect Dis, 14 (4), 170-177. doi:10.5455/JMID.20240823100803 Turabian Style Cimen, Nurcan, and Mehtap Sonmez. 2024. Hospital candidemia infection and related factors in intensıve care units. Journal of Microbiology and Infectious Diseases, 14 (4), 170-177. doi:10.5455/JMID.20240823100803 Chicago Style Cimen, Nurcan, and Mehtap Sonmez. "Hospital candidemia infection and related factors in intensıve care units." Journal of Microbiology and Infectious Diseases 14 (2024), 170-177. doi:10.5455/JMID.20240823100803 MLA (The Modern Language Association) Style Cimen, Nurcan, and Mehtap Sonmez. "Hospital candidemia infection and related factors in intensıve care units." Journal of Microbiology and Infectious Diseases 14.4 (2024), 170-177. Print. doi:10.5455/JMID.20240823100803 APA (American Psychological Association) Style Cimen, N. & Sonmez, . M. (2024) Hospital candidemia infection and related factors in intensıve care units. Journal of Microbiology and Infectious Diseases, 14 (4), 170-177. doi:10.5455/JMID.20240823100803 |