| Research Article Online Published: 27 Dec 2024 | ||
J Microbiol Infect Dis. 2024; 14(4): 191-193 J. Microbiol. Infect. Dis., (2024), Vol. 14(4): 191–193 Research Article Intra-familial transmission dynamics of Hepatitis B VirusP.A.S.R. Paththamperuma, R.G.L.S. Rajamanthri, T.T. Pattiyakumbura* and M.A.R.V. MuthugalaDepartment of Virology, National Hospital Kandy, Kandy, 20000, Sri Lanka *Corresponding Author: T. T. Pattiyakumbura.Department of Virology, National Hospital Kandy, Kandy, 20000, Sri Lanka. Email: thulanipattiyakumbura [at] yahoo.com Submitted: 10/07/2024 Accepted: 21/11/2024 Published: 31/12/2024 © 2024 Journal of Microbiology and Infectious Diseases
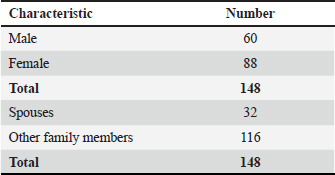
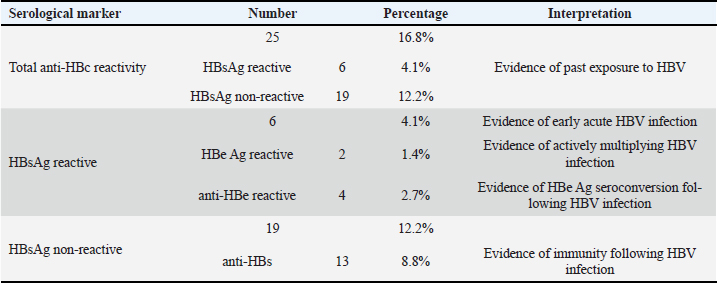
ABSTRACTIntroduction: Hepatitis B is a liver infection caused by the Hepatitis B Virus (HBV). Sri Lanka is considered a country of low endemicity, with an HBV infection prevalence estimated at less than 2%. However, there is a high risk of HBV transmission among family members and close contacts of infected patients. Preventing intra-familial transmission is crucial in managing Hepatitis B. This study aimed to evaluate the HBV infection status among family contacts of HBV-infected patients followed up at the National Hospital, Kandy, Sri Lanka. Methods: Laboratory data on serological markers from 148 family contacts of 42 index cases were analyzed. All index cases were followed up at the Department of Virology at the National Hospital, Kandy, after being referred from gastroenterology, Sexually Transmitted Diseases (STD), and medical clinics. Serum samples from the close contact of family members of these index cases were tested for HBV serological markers between March 2017 and February 2021. Results: Out of the 148 family members, 25 (16.89%) showed evidence of exposure to HBV (reactive anti-HBc) at the time of screening. Six family members (4.1%) were positive for HBsAg. Among these, two had evidence of active infection (reactive HBeAg/non-reactive anti-HBe) and four had seroconverted to anti-HBe. Among exposed contacts, 19/25 (12.8%) were non-reactive for HBsAg, indicating past infection, of whom 13/25 (8.7%) were positive for anti-HBs indicating immunity following infection. Among 32 spouses, six (18.75%) showed evidence of exposure to HBV infection. In two index cases, all family members had evidence of HBV infection. Thirty-six (24.3%) family members had taken the HBV vaccine prior to screening. Among them, 26 (17.6%) showed adequate immunity against Hepatitis B (anti-HBs antibody titer > 10 mIU/ml), and all were negative for anti-HBc, indicating immunity following vaccination. Conclusion: The HBV infection rate among family members (16.9%) is significantly higher than in the general population (<2%). Understanding the transmission dynamics of intrafamilial HBV infection is crucial for identifying high-risk family members, guiding targeted vaccination strategies, facilitating early diagnosis and monitoring, and preventing vertical transmission. Effective measures for preventing intrafamilial transmission of HBV include contact screening, vaccinating non-immune family members, providing health education, and counseling family members on transmission risks and preventive behaviors. These interventions play a pivotal role in reducing the spread of HBV within families and mitigating the long-term health consequences of chronic infection. Keywords: Hepatitis B Virus (HBV), Intra-familial, Transmission, Hepatitis B infection. INTRODUCTIONHepatitis B, caused by the Hepatitis B virus (HBV), is a significant global public health concern due to its potential to cause acute and chronic hepatitis, leading to serious liver conditions like cirrhosis and hepatocellular carcinoma (Hepatitis, 2021). It remains a leading cause of end-stage liver disease worldwide (Mandell, 2000; Centers for Disease Control and Prevention, 2022). In 2019 alone, approximately 296 million people were living with chronic HBV infection, with 1.5 million new infections and 820,000 deaths attributed to Hepatitis B that year (Hepatitis, 2021). The main routes of HBV transmission include parenteral exposure (through blood and body fluids), sexual contact, vertical transmission (from mother to child), and horizontal transmission (among close contacts) hence family members and close contact with infected individuals face a significant risk of transmission (Hepatitis, 2021; Mandell, 2000; Kashiwagi et al., 1985; Muthugala and Galagoda, 2015; Centers for Disease Control and Prevention, 2023). In Sri Lanka, the exact incidence and prevalence of Hepatitis B in the general population are not well documented. Still, they are estimated to be less than 2%, classifying the country as having low endemicity (Noordeen et al., 2015; Samaraweera, 2017). However, various studies globally, including those conducted in Sri Lanka, have reported a significant incidence of HBV infection among family members and close contacts (Kashiwagi et al., 1985; Muthugala and Galagoda, 2015; Sofian et al., 2016). Understanding how HBV spreads within families is crucial for its control and prevention, however, data on such populations remain limited in Sri Lanka. Therefore, we conducted this study to assess the HBV infection status among family contacts of HBV-infected patients at the Department of Virology, National Hospital Kandy, aiming to contribute to the understanding and management of Hepatitis B transmission dynamics. Table 1. Demographic data of the study population
MATERIALS AND METHODSLaboratory data on Hepatitis B viral serological markers were collected and analyzed for 148 family contacts of 42 index cases from March 2017 to February 2021. The index cases were patients who were HBVDNA positive and were followed up at the Department of Virology, National Hospital Kandy, Sri Lanka. Family members of these patients who had been referred for contact screening have been included in this study. The serological markers analyzed in the study population included Hepatitis B surface antigen (HBsAg), Hepatitis B core IgM (anti-HBc IgM), Hepatitis B core total antibody (anti-HBc total Ab), Hepatitis B e antigen (HBeAg), Hepatitis B e antibody (anti-HBe), and Hepatitis B surface antibody (anti-HBs). All these markers were tested using commercially validated immunoassays. Table 2. Hepatitis B viral serological markers among family contacts.
RESULTS1. Analysis of demographic dataData from 148 family contacts of 42 index cases were analyzed (Table 1). Among the family contacts, 88 (59.46%) were females and 60 (40.54%) were males. Of the screened family members, 32 (21.62%) were spouses, and 116 (78.38%) were other family members (children, parents, siblings). 2. Analysis of serological markers and vaccination status among family contactsOut of 148 specimens analyzed, 25 (16.8%) showed evidence of horizontal transmission of HBV among family members with anti-HBc reactivity. Among these, 6 (4.1%) tested reactive for HBsAg, while 19(12.2%) specimens were non-reactive for HBsAg. Of the HBsAg-reactive 6 specimens, 2 were reactive for HBeAg, indicating actively multiplying infection and 4 were reactive for anti-HBe, indicating seroconversion. Among the 19 specimens that were negative for HBsAg, 13 specimens showed anti-HBs reactivity indicating immunity following HBV infection. Six (18.75%) out of 32 spouses and 19 (16.37%) of other family members showed evidence of HBV infection. In two index cases, all family members were affected, and in 12 (28.57%) index cases, at least one family member was affected (Table 2). DISCUSSIONThis study found a higher Hepatitis B infection rate (16.8%) among family members compared to the general population. This highlights that close family members are more exposed to the infection than the general population. A study conducted in 2015 in Sri Lanka showed an infection rate of 23.9% among family members (Muthugala and Galagoda, 2015). The lower rates observed in this study could be attributed to awareness programs, active tracing of close contacts, vaccination of high-risk individuals, and improvements in diagnostics and management of HBV infection. Among the 36 individuals who had been vaccinated before screening, 28 (77.78%) were children under 12 years old, vaccinated through the National Immunization Programme (NIP) in Sri Lanka. Since vaccination is the most effective way to prevent HBV, the inclusion of HBV vaccination in the national immunization program in 2003 has been a successful measure in preventing HBV transmission. However, adolescents and adults who were not vaccinated through NIP and are at high risk for HBV infection need to be actively traced and vaccinated. A proper understanding of the transmission dynamics of intra-familial HBV infection is crucial for preventing HBV infection among family contacts. Effective measures for preventing intra-familial transmission include contact screening, vaccinating non-immune family members, and providing health education and counseling to family members (Muthugala and Galagoda, 2015; Sofian et al., 2016). There are a few limitations to this study. Index cases were selected based on their presentation for diagnostic testing and might not be the first cases within their families. Additionally, molecular and biochemical markers were not evaluated in this study. Future large-scale, multi-center studies are needed to better understand the transmission kinetics of HBV infection. AUTHOR CONTRIBUTIONThe study was conducted and the data was analyzed by P.A.S.R. Paththamperuma, T.T. Pattiyakumbura, and R.G.L.S. Rajamanthrie under the supervision of M.A.R.V. Muthugala. The manuscript was drafted by P.A.S.R Paththamperuma and T.T. Pattiyakumbura and reviewed by M.A.R.V. Muthugala. All authors approved the final manuscript. CONFLICT OF INTERESTSThe authors declared that there are no conflicts of interest. FUNDINGNo external funding source. ETHICAL CLEARANCEThis is not applicable as it is laboratory data analysis. Permission to publish the laboratory data was obtained from the Director of the National Hospital Kandy, Sri Lanka. ACKNOWLEDGMENTSThe authors acknowledge the staff at the Regional Virology Laboratory and Infection Control Unit, National Hospital, Kandy, Sri Lanka. REFERENCESCenters for Disease Control and Prevention (CDC). (2023). Hepatitis B. Retrieved June 26, 2023, from https://www.cdc.gov/hepatitis/hbv/index.htm Centers for Disease Control and Prevention. 2023. Hepatitis B | CDC. Available via https://www.cdc.gov/hepatitis/hbv/index.htm (Accessed 26 June 2023) Hepatitis B. 2021. Available via https://www.who.int/news-room/fact - sheets/detail/hepatitis-b Kashiwagi, S., Hayashi, J., Nomura, H., Ikematsu, H. and Kajiyama, W. 1985. Large–scale survey of hepatitis B virus infection in families. Microbiol Immunol 29(10), 951–958. Mandell, G.L. 2000. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 9th edition. Muthugala, M a. R.V. and Galagoda, G.C.S. 2015. Transmission of hepatitis B virus infection among family contacts of chronic hepatitis B carriers in Sri Lanka. Sri Lankan J Infect Diseases 5(2), 58–63. Noordeen, F., Pitchai, F.N.N. and Rafeek, R.A. 2015. A review of hepatitis B virus infection in Sri Lanka. Sri Lankan J Infect Diseases 5(2), 42–50. Samaraweera, D. S. (2017). Update on Hepatitis B and C. Epidemiology Unit Weekly Epidemiological Report, 44(45), 4. Retrieved from https://www.epid.gov.lk/storage/post/pdfs/vol_44_no_45-english.pdf Sofian, M., Banifazl, M., Ziai, M., Aghakhani, A., Farazi, A.A. and Ramezani, A. 2016. Intra-familial Transmission of Hepatitis B Virus Infection in Arak, Central Iran. Iran J Pathol 11(4), 328–333. | ||
| How to Cite this Article |
| Pubmed Style Paththamperuma S, Rajamanthri L, Pattiyakumbura T, Muthugala R. Intra-familial transmission dynamics of Hepatitis B Virus. J Microbiol Infect Dis. 2024; 14(4): 191-193. doi:10.5455/JMID.20240710075307 Web Style Paththamperuma S, Rajamanthri L, Pattiyakumbura T, Muthugala R. Intra-familial transmission dynamics of Hepatitis B Virus. https://www.jmidonline.org/?mno=209202 [Access: January 07, 2026]. doi:10.5455/JMID.20240710075307 AMA (American Medical Association) Style Paththamperuma S, Rajamanthri L, Pattiyakumbura T, Muthugala R. Intra-familial transmission dynamics of Hepatitis B Virus. J Microbiol Infect Dis. 2024; 14(4): 191-193. doi:10.5455/JMID.20240710075307 Vancouver/ICMJE Style Paththamperuma S, Rajamanthri L, Pattiyakumbura T, Muthugala R. Intra-familial transmission dynamics of Hepatitis B Virus. J Microbiol Infect Dis. (2024), [cited January 07, 2026]; 14(4): 191-193. doi:10.5455/JMID.20240710075307 Harvard Style Paththamperuma, S., Rajamanthri, . L., Pattiyakumbura, . T. & Muthugala, . R. (2024) Intra-familial transmission dynamics of Hepatitis B Virus. J Microbiol Infect Dis, 14 (4), 191-193. doi:10.5455/JMID.20240710075307 Turabian Style Paththamperuma, Sachika, Lakmali Rajamanthri, Thulani Pattiyakumbura, and Rohitha Muthugala. 2024. Intra-familial transmission dynamics of Hepatitis B Virus. Journal of Microbiology and Infectious Diseases, 14 (4), 191-193. doi:10.5455/JMID.20240710075307 Chicago Style Paththamperuma, Sachika, Lakmali Rajamanthri, Thulani Pattiyakumbura, and Rohitha Muthugala. "Intra-familial transmission dynamics of Hepatitis B Virus." Journal of Microbiology and Infectious Diseases 14 (2024), 191-193. doi:10.5455/JMID.20240710075307 MLA (The Modern Language Association) Style Paththamperuma, Sachika, Lakmali Rajamanthri, Thulani Pattiyakumbura, and Rohitha Muthugala. "Intra-familial transmission dynamics of Hepatitis B Virus." Journal of Microbiology and Infectious Diseases 14.4 (2024), 191-193. Print. doi:10.5455/JMID.20240710075307 APA (American Psychological Association) Style Paththamperuma, S., Rajamanthri, . L., Pattiyakumbura, . T. & Muthugala, . R. (2024) Intra-familial transmission dynamics of Hepatitis B Virus. Journal of Microbiology and Infectious Diseases, 14 (4), 191-193. doi:10.5455/JMID.20240710075307 |