| Case Report | ||
J Microbiol Infect Dis. 2023; 13(3): 168-170 J. Microbiol. Infect. Dis., (2023), Vol. 13(3): 168–170 Case Report Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case reportGashaw Solela* and Alazar SitotawDepartment of Internal Medicine, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia *Corresponding Author: Gashaw Solela. Department of Internal Medicine, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia. Email: gashawsol [at] gmail.com Submitted: 25/07/2023 Accepted: 17/09/2023 Published: 30/09/2023 © 2023 Journal of Microbiology and Infectious Diseases
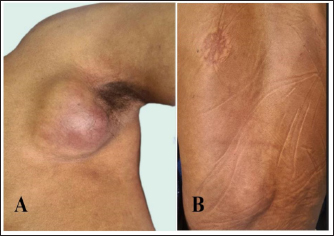
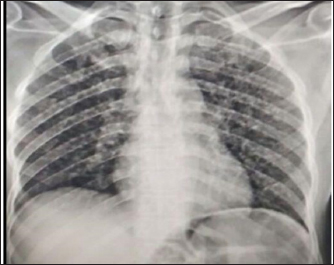
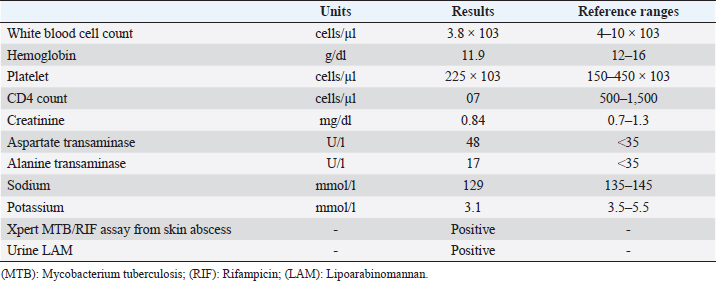
AbstractBackground: Cutaneous tuberculosis (TB) is rare, constituting only 2% of all cases of TB. Metastatic tuberculous abscesses typically result from the Bacillus spreading hematogenously from the main site of infection to the subcutaneous tissue when the body’s cellmediated immunity is compromised and present with one or more non-tender and fluctuant subcutaneous nodules. Case Description: A 51-year-old male presented with a dry cough of 1 month duration associated with vomiting, loss of appetite, and easy fatigability. He had left armpit and lower back skin swellings of similar duration. Findings were whittish coat over the dorsal part of the tongue, crepitation over the lower 2/3rd of the bilateral posterior chest, non-tender fluctuant masses over the left axilla and lower back. Chest X-ray showed multiple bilateral air space nodules and abdominopelvic U/S showed numerous hypoechoic splenic lesions. Urine lipoarabinomannan (LAM) and Xpert MTB/RIF assay from the axillary skin abscess were positive. He was started on antituberculous therapy and showed marked improvement after a month of follow up. Conclusion: It is worth considering the uncommon manifestations of tuberculosis including metastatic skin abscesses in the appropriate clinical context, to avoid misdiagnosis and underreporting in high tuberculosis burden countries. We strongly advise the utilization of Xpert MTB/RIF assay and/or urine lipoarabinomannan for the diagnosis of different forms of tuberculosis including cutaneous TB in HIV positive patients, especially in the absence of sputum for microbiologic tests, like in our patient. Keywords: Disseminated tuberculosis, Cutaneous tuberculosis, Metastatic skin abscesses, Immunocompromised patient. IntroductionDisseminated tuberculosis (TB) is characterized by the presence of two or more noncontiguous sites caused by hematogenous dissemination of Mycobacterium TB, occurring as a result of progressive primary infection or reactivation of a latent focus with subsequent spread (Khan et al., 2016). Even when the typical pathologic or radiologic findings are missing, miliary TB refers to progressive and widely disseminated forms of TB, and it is quite similar to disseminated TB (Salvado et al., 2002). The typical extra-pulmonary TB locations include lymph nodes, pleura, genito-urinary tract, bones, joints, meninges, and peritoneum (Gopal et al., 2000). Cutaneous TB, which is extremely uncommon, constitutes about 2% of all TB cases (Semaan et al., 2008). Patients with metastatic tuberculous abscesses manifest with one or more non-tender, fluctuant, subcutaneous nodules that eventually pierce the skin and give rise to ulcers and draining sinuses (Singal et al., 2022). We have reported the case of a patient diagnosed with disseminated TB with metastatic skin tuberculous abscesses on the background of advanced immunosuppression due to retroviral infection. Case DetailsA 51-year-old male presented with a dry cough of 1 month duration associated with occasional vomiting of ingested matter, loss of appetite, and easy fatigability. He had left armpit and lower back skin swellings of similar duration. He has a history of alcohol consumption of significant amount for 20 years. He tested positive for human immunodeficiency virus (HIV) a week before his current presentation. He has no history of loss of consciousness, abnormal body movement, or neck stiffness. He had no known chronic medical illness. Physical examination revealed blood pressure of 95/60 mmHg, pulse rate of 78 beats per minute, respiratory rate of 20 breaths per minute, temperature of 36°C, oxygen saturation of 95% with room air, whitish coat over the dorsal part of the tongue, crepitation over the lower 2/3rd of bilateral posterior chest, 4 cm by 4 cm non-tender fluctuant mass over the left axilla and 2 cm by 4 cm non-tender, fluctuant mass over the lower back (Fig. 1). Upon investigation, chest X-ray showed multiple bilateral air space nodules (Fig. 2); abdominopelvic U/S showed numerous hypoechoic splenic lesions; complete blood count was non-remarkable; urine lipoarabinomannan (LAM) was positive, and Xpert MTB/RIF assay from the left axillary skin abscess was positive for rifampicin sensitive Mycobacterium tuberculosis (Table 1). Having all those evidences of disseminated TB involving the lung, spleen, and skin, the skin abscesses were drained and the patient was started on anti-tuberculous medications with pyridoxine. He also received fluconazole for oral and esophageal candidiasis. After a week of anti-TB initiation, he was started on highly active antiretroviral therapy. He showed marked improvement after a month of anti-tuberculous therapy.
Fig. 1. Non-tender fluctuant axillary mass measuring 4 cm by 4 cm (A), 2 cm by 4 cm nontender, fluctuant mass over the lower back area (B).
Fig. 2. Chest X-ray revealed multiple bilateral air space nodules. Ethical approvalThe case report meets ethical guidelines and adheres to the local legal requirements. DiscussionDissemination of Mycobacterium TB can happen due to a progressive primary infection or the reactivation of a latent focus followed by lymphohematogenous spread. The exact method by which this happens, meanwhile, is unclear (Krishnan et al., 2010). Inflammatory papules, verrucous plaques, suppurative nodules, chronic ulcers, and other lesions can all be seen in the clinical presentation of cutaneous TB (Lai-Cheong et al., 2007). Metastatic tuberculous abscesses, also known as tuberculous gummas, are rare forms of TB that make up 1%–2% of all cutaneous TB cases (Machan et al., 2018). These are multibacillary forms of cutaneous TB, typically developing when there is a reduction in cell-mediated immunity, which allows the spread of the bacillus hematogenously from the major focus of infection to the subcutaneous tissue (Barbagallo et al., 2002). There is a wide range of clinical presentations of metastatic tuberculous abscesses depending on the organism’s virulence, the route of infection, and the level of immunity of the vulnerable host. The frequent characteristics are defined as single or multiple, painful, cold abscesses with ulceration or fistulae (Almagro et al., 2005) like the present case. Tuberculous gummas most frequently affect the limbs, particularly the thighs and buttocks (Machan et al., 2018) unlike our patient where the axilla and back were mainly involved. Three-fourths of similar cases involve associated sites and the most frequent ones are the lung, lymph nodes, and musculoskeletal system (Machan et al., 2018) unlike our patient, where the lungs and spleen were the associated sites of involvement. One major differential diagnosis of cutaneous TB is scrofuloderma, which has similar clinical and histologic characteristics to metastatic tuberculous abscesses. Scrofuloderma develops as a continuous extension of an infection from an underlying tuberculous focus instead of hematogenous spread (Almagro et al., 2005). The chest X-ray findings suggestive of pulmonary TB and the absence of scrofula, were against scrofuloderma. The cutaneous manifestations in metastatic skin abscesses are most likely due to the result of hematogenous spread of Mycobacterium tuberculous bacteria. Though, there is no chemotherapeutic regimen and duration that is universally recommended for the treatment of metastatic tuberculous abscesses, the typical regimen, 2RHZE/4RH, which is used in the treatment of pulmonary TB, is very effective for the treatment of cutaneous TB (Machan et al., 2018). Similar to a 56-year-old Bangladeshi man who presented with numerous skin abscesses all over his body and responded to anti-TB treatment after a month of starting anti-tubercular therapy, marked improvement was seen in our patient after a month of anti-TB (Alam et al., 2021). Table 1. Summary of laboratory results.
ConclusionIt is worth considering the uncommon manifestations of tuberculosis including metastatic skin abscesses in the appropriate clinical context, to avoid misdiagnosis and underreporting in high tuberculosis burden countries. We strongly advise the utilization of Xpert MTB/RIF assay and/or urine lipoarabinomannan for the diagnosis of different forms of tuberculosis including cutaneous TB in HIV positive patients, especially in the absence of sputum for microbiologic tests, like in our patient. Data availabilitySupporting data is available with the corresponding author upon a reasonable request. Authors’ contributionsGS was involved in the conceptualization of the case report and prepared the initial draft of the manuscript. AA was involved in the revision of the initial manuscript. Both authors read and approved the final manuscript. ReferencesAlam, M.A., Ahmed, M.N., Khan, A.H. and Arafat, S.M. 2021. Metastatic tuberculous abscess: a rare manifestation of cutaneous tuberculosis. IDCases 26, e01257. Almagro, M., Del Pozo, J., Rodríguez-Lozano, J., Silva, J.G., Yebra-Pimentel, M.T. and Fonseca, E. 2005. Metastatic tuberculous abscesses in an immunocompetent patient. Clin. Exp. Dermatol. Clin. Dermatol. 30(3), 247–249. Barbagallo, J., Tager, P., Ingleton, R., Hirsch, R.J. and Weinberg, J.M. 2002. Cutaneous tuberculosis: diagnosis and treatment. Am. J. Clin. Dermatol. 3(5), 319–328. Gopal, R., Padmavathy, B.K., Vasanthi, S. and Jayashree, K. 2000. Extra pulmonary tuberculosis—a retrospective study. Ind. J. Tub. 47, 245. Khan, F.Y., Dosa, K., Fuad, A., Ibrahim, W., Alaini, A., Osman, L., Albadri, M. and Yassin, M.A. 2016. Disseminated tuberculosis among adult patients admitted to Hamad general hospital, Qatar: a five year hospital based study. Mycobact. Dis. 6, 212. Krishnan, N., Robertson, B.D. and Thwaites, G. 2010. The mechanisms and consequences of the extrapulmonary dissemination of Mycobacterium tuberculosis. Tuberculosis (Edinb) 90(6), 361–366. Lai-Cheong, J.E., Perez, A., Tang, V., Martinez, A., Hill, V. and Menagé Hdu, P. 2007. Cutaneous manifestations of tuberculosis. Clin. Exp. Dermatol. 32(4), 461–466; doi: 10.1111/j.1365-2230.2007.02352.x. Machan, A., Hanafi, T., Hjira, N. and Boui, M. Tuberculous gummas: epidemiological, clinical, bacteriological, immunological, and therapeutic features. Int. J. Mycobacteriol.7(3), 203–211. Salvado, G., Santos, C., André, M., Gomes, C., Diogo, N. and Marques, M. 2002. Miliary tuberculosis. Rev. Port. Pneumol. 8, 315–327. Semaan, R., Traboulsi, R. and Kanj, S. 2008. Primary Mycobacterium tuberculosis complex cutaneous infection: report of two cases and literature review. Int. J. Infect. Dis. 12(5), 472–477. Singal, A., Kaur, I., Jakhar, D., Pandhi, D., Grover, C. and Gandhi, V. 2022. Clinicoepidemiological characteristics of cutaneous tuberculosis in 1458 Indian patients: a retrospective analytical study from a tertiary care center. Int. J. Dermatol. 61(8), 1012–1022. | ||
| How to Cite this Article |
| Pubmed Style Solela G, Sitotaw A. Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. J Microbiol Infect Dis. 2023; 13(3): 168-170. doi:10.5455/JMID.2023.v13.i3.10 Web Style Solela G, Sitotaw A. Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. https://www.jmidonline.org/?mno=158287 [Access: January 25, 2026]. doi:10.5455/JMID.2023.v13.i3.10 AMA (American Medical Association) Style Solela G, Sitotaw A. Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. J Microbiol Infect Dis. 2023; 13(3): 168-170. doi:10.5455/JMID.2023.v13.i3.10 Vancouver/ICMJE Style Solela G, Sitotaw A. Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. J Microbiol Infect Dis. (2023), [cited January 25, 2026]; 13(3): 168-170. doi:10.5455/JMID.2023.v13.i3.10 Harvard Style Solela, G. & Sitotaw, . A. (2023) Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. J Microbiol Infect Dis, 13 (3), 168-170. doi:10.5455/JMID.2023.v13.i3.10 Turabian Style Solela, Gashaw, and Alazar Sitotaw. 2023. Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. Journal of Microbiology and Infectious Diseases, 13 (3), 168-170. doi:10.5455/JMID.2023.v13.i3.10 Chicago Style Solela, Gashaw, and Alazar Sitotaw. "Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report." Journal of Microbiology and Infectious Diseases 13 (2023), 168-170. doi:10.5455/JMID.2023.v13.i3.10 MLA (The Modern Language Association) Style Solela, Gashaw, and Alazar Sitotaw. "Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report." Journal of Microbiology and Infectious Diseases 13.3 (2023), 168-170. Print. doi:10.5455/JMID.2023.v13.i3.10 APA (American Psychological Association) Style Solela, G. & Sitotaw, . A. (2023) Uncommon manifestation of disseminated tuberculosis with metastatic skin abscesses in an immunocompromised adult patient: A case report. Journal of Microbiology and Infectious Diseases, 13 (3), 168-170. doi:10.5455/JMID.2023.v13.i3.10 |