| Case Report | ||
J. Microbiol. Infect. Dis., (2025), Vol. 15(1): 32–35 Case Report Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challengeSurafel Nadew Firdawoke1*, Abdi Dandena Dibaba2, Abera Kuma Begna1, Selam Hagos Gebrewahd3 and Samrawit Gizaw11Department of Internal Medicine, Faculty of Medical Science, Hawassa University, Awasa, Ethiopia 2Department of Radiology, Faculty of Medical Science, Institute of Health, Jimma University, Jimma, Ethiopia 3Pediatrics Unit, Ethiopian Armed Force Comprehensive Hospital, Addis Ababa, Ethiopia *Corresponding Author: Surafel Nadew Firdawoke. Department of Internal Medicine, Faculty of Medical Science, Hawassa University, Awasa, Ethiopia. Email: nasewsurafel [at] yahoo.com Submitted: 11/12/2024 Accepted: 30/01/2025, Published: 31/03/2025 © 2025 Journal of Microbiology and Infectious Diseases
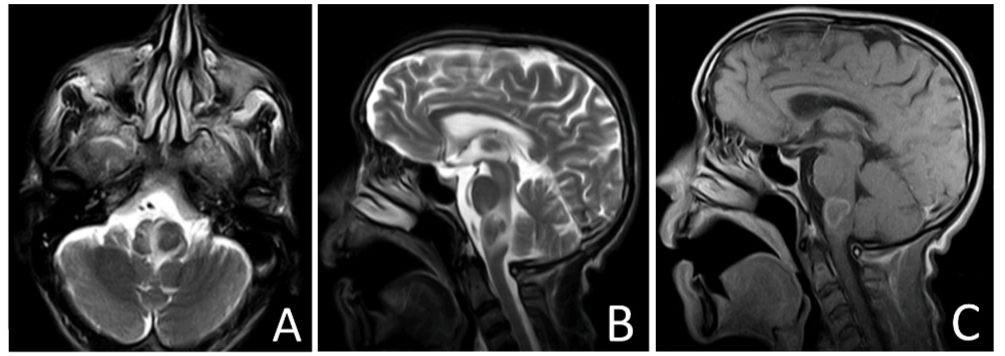
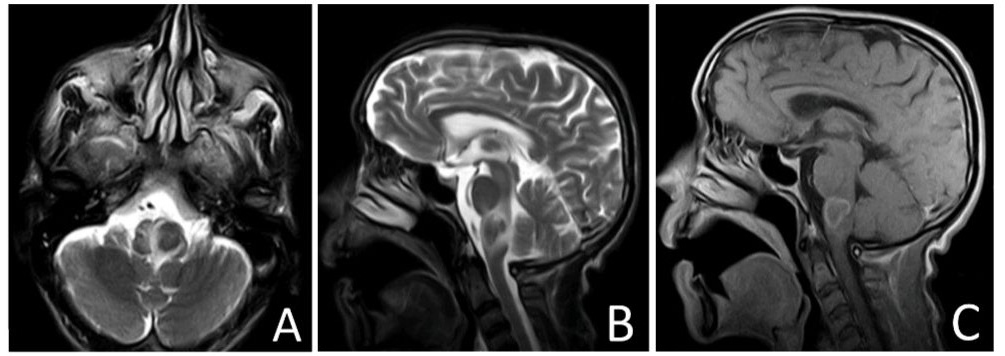
ABSTRACTBackground: Tuberculosis (TB) remains a major global health concern, with central nervous system (CNS) TB being a rare but serious form associated with high morbidity and mortality. Early diagnosis is crucial because symptoms can overlap with other conditions. Case Presentation: A 38-year-old male presented with progressive dysphagia, vomiting, and weight loss. Initial investigations suggested gastrointestinal issues, but further neurological evaluation revealed ataxia. Magnetic Resonance Imaging (MRI) revealed a Tuberculoma in the right lateral medulla, causing the lateral medullary syndrome. The patient was started on anti-TB treatment and showed significant improvement, with lesion resolution after 12 months. Discussion: CNS TB can present with nonspecific symptoms, making diagnosis challenging. In this case, the tuberculoma caused dysphagia by affecting the cranial nerves involved in swallowing. Early diagnosis and imaging are vital for timely treatment. Conclusion: This case highlights the importance of considering CNS TB in patients with unexplained swallowing difficulties, particularly in TB-endemic regions, to ensure prompt treatment and better outcomes. Keywords: Dysphagia, Tuberculosis, Central nervous system, Diagnosis, Prognosis. IntroductionTuberculosis (TB) is an infectious disease that remains a major global public health concern. TB is particularly concerning in Africa which, accounts, for nearly a fourth (24%) of the total global burden in incident cases as reported by the WHO in its 2023 report (World Health Organization, 2023). Ethiopia is among the 30 countries with a higher burden of TB, with these countries accounting for nearly 86% of the Global TB burden (Alene et al., 2023). Central nervous system (CNS) TB is among the rare forms of extrapulmonary TB, which accounts for approximately 1% of all extra pulmonary TB (Abbasi et al., 2021). CNS TB is associated with a high degree of Morbidity and mortality and requires a high index of suspicion for early diagnosis and treatment (Alharbi et al., 2021). The clinical symptoms of CNS TB can be nonspecific and depend on the location and number of lesions. The symptoms could range from headache, mmeningismus, altered mentation, seizure, focal neurological deficit, and coma being common examples. Neuroimaging is often employed in suspected cases of CNS TB and can have varying characteristics that may overlap with other infectious and noninfectious pathologies. Imaging appearance depends on the location of the lesion and maturation stage; hence, it is very important to be aware of the common imaging appearance of CNS TB. ObjectiveTo show the diagnostic challenges of common disease like TB when it presented with an unusual presentation like Disphagia as in our case. Case PresentationFirst visitA 38-year-old man presented to the emergency department with progressive difficulty swallowing over the past 2 months, which has limited the swallowing of solids, semi solids as well as liquids. The patient also had multiple episodes of nonprojectile vomiting and exhibited significant unquantified weight loss. The patient had a long-standing history of dyspeptic symptoms and was, previously managed with proton pump inhibitors and oral antibiotics during several hospital visits over the years. He denied any history of alcohol use, smoking, distention, respiratory issues, urinary problems, or other significant medical or surgical history. Upon physical examination, the patient appeared acute or chronic illness and appeared to arrive at the outpatient department supported on a stretcher. His vital signs were stable: pulse rate, 86 beats/min, respiratory rate, 12 breaths/min; temperature, 37.1°C and blood pressure, and 126/86 mm Hg. Head ear nose and throat, cardiac, chest, abdominal, musculoskeletal, and CNS examinations were unremarkable. A full neurological examination was not performed due to the patient’s condition, and the initial assessment was unremarkable. Laboratory tests, including Complete Blood Count, electrolytes, organ function tests, and Human Immunodeficiency Virus (HIV) tests, were all normal. An upper Gastrointestinal endoscopy was performed due to the suspicion of an esophageal neoplasm, but only mild features of reflux disease were found, with no obstructive lesions. After overnight resuscitation, the patient was referred to an external diagnostic center for a chest computed tomography (CT) scan to check for extra luminal compression as a potential cause of dysphagia (Dysphagia lusoria). Second visitDuring the second visit, a chest CT report was obtained, which showed no extra luminal compression of the esophagus (Fig. 1). Clinically, the patient showed improvement and no longer needed stretcher assistance. A full neurological examination revealed an ataxic gait. The patient was asked to demonstrate swallowing difficulty with a bedside water drinking challenge, which indicated difficulty initiating swallowing, suggesting neurological pharyngeal dysphagia. Mild weakness was also noted. A postcontrast magnetic resonance imaging (MRI) revealed a well-defined T2 hypointense lesion in the right lateral medulla with minimal surrounding edema. The lesion showed peripheral enhancement on post contrast imaging, indicating a tuberculoma causing lateral medullary syndrome. The patient was started on anti-TB medication (Fig. 1). Treatment and outcomeAt the 2-month follow-up, the patient showed significant improvement in dysphagia, nausea, and vomiting. Subsequent visits improved gait and balance. A follow-up MRI at 12 months after completing the antituberculosis regimen showed complete resolution of the lesion in the lateral medulla (Fig. 2).
Fig. 1. Axial T2 (A), Sagittal T2 (B) and Sagittal (T1 post contrast) images of the brain showing a well-defined T2 hypo intense peripherally enhancing lesion in the left lateral medulla with surrounding edema seen.
Fig. 2. Axial T2 (A), Sagittal T2 (B) and Sagittal (T1 post contrast) images of the brain taken after 9 months of anti TB medication showing a complete resolution of the medullary lesion. DiscussionCNS TB can present as TB meningitis, intracranial tuberculoma, or tuberculous abscess, each posing significant health challenges due to high associated mortality and morbidity (Schaller et al., 2019). Intracranial tuberculomas, resulting from hematogenous dissemination of Mycobacterium TB, are rare. They are typically located in the front parietal region or basal ganglia but can also appear in more unusual sites like the brainstem (Perez-Malagon et al., 2021). The increasing incidence of intracranial tuberculomas is partly attributed to rising rates of HIV infection and immigration from TB-endemic areas (C.B. IJsselmuiden and Faden, 2011). The absence of systemic TB symptoms in >50% of CNS TB cases often leads to delayed diagnoses, compounded by variable clinical presentations (Rangel Guerra et al., 1991). Brainstem tuberculomas, which represent 1%–2% of all TB cases, pose significant diagnostic challenges because of their deep location, which limits the feasibility of biopsy (Thakur et al., 2018). Symptoms often include nonspecific manifestations, such as headache, seizure, and motor weakness. In some cases, patients may exhibit atypical symptoms like dysphagia, further complicating the diagnostic process (Chin, 2019). The potential delay in identifying CNS TB emphasizes the necessity for increased clinical vigilance, particularly in patients from TB-endemic regions or those with known risk factors, such as HIV (Seputra et al., 2023). This case report illustrates the critical link between intracranial tuberculomas and dysphagia. The dysphagia was primarily attributed to the involvement of the cranial nerves responsible for swallowing, which was influenced by the tuberculoma's impact on the medullary region. The lesion in the right lateral medulla disrupted the neural pathways crucial for coordinated swallowing, resulting in neurological pharyngeal dysphagia. The relationship between lateral medullary syndrome, also known as Wallenberg syndrome, and dysphagia highlights the importance of CNS TB in patients with swallowing difficulties. The initial presentation of the patient included progressive dysphagia, nonprojectile vomiting, and weight loss, which could have easily been mistaken for gastrointestinal disorders, such as esophageal neoplasm and reflux disease. The standard investigation revealed mild reflux disease, which failed to address the underlying neurological cause. Follow-up visits revealed neurological signs, including an ataxic gait, which led to further imaging with MRI, ultimately revealing a well-defined lesion in the right lateral medulla. The significant improvement observed following the initiation of anti-TB therapy underscores the importance of including CNS TB in the differential diagnosis of patients with unexplained dysphagia, especially in regions where TB is endemic. This case is a reminder of the importance of a comprehensive approach in the evaluation of patients with unexplained neurological symptoms and swallowing difficulties. Early recognition and appropriate imaging can facilitate timely intervention, thereby improving patient outcomes. ConclusionThis case highlights the diagnostic challenges associated with intramedullary TB leading to dysphagia and underscores the need for heightened clinical awareness regarding the potential manifestations of CNS TB. A thorough understanding of these connections can improve diagnostic accuracy and enhance patient management, ultimately leading to better health outcomes. AcknowledgmentWe thank our patient for permitting us to write this case report. FundingNo specific grant from funding organizations in the public private, or nonprofit sectors has been provided for this study. Ethical issueThe patient provided written informed consent for publication of this case, and case-specific information and images were included in the consent form. This institution does not require ethical approval for the publication of a single case report. ReferencesAbbasi, F., Ozer, M., Juneja, K., Goksu, S.Y., Mobarekah, B.J. and Whitman, M.S. 2021. Intracranial tuberculoma mimicking neurosarcoidosis: a clinical challenge. Infect. Dis. Rep. 13(1), 181–186. Alene, K.A., Python, A., Weiss, D.J., Elagali, A., Wagaw, Z.A., Kumsa, A., Gething, P.W. and Clements, A.C. 2023. Mapping tuberculosis prevalence in Ethiopia using geospatial meta-analysis. Int. J. Epidemiol. 52(4), 1124–1136. Alharbi, A., Khairy, S., Al Sufiani, F. and Alkhani, A. 2021. Intracranial tuberculomas: a case report of clinical, radiological, and pathological characteristics. Int. J. Surg. Case. Rep. [Internet]. 88(August), 106477; doi: 10.1016/j.ijscr.2021.106477 Ijsselmuiden, C. B. and R.R. Faden The New England Journal of Medicine, 2011. Downloaded from nejm.org on January 31, 2011. 1992;326. Chin, J.H. 2019. Neurotuberculosis: a clinical review. Semin. Neurol. 39, 456–461. Perez-Malagon, C.D., Barrera-Rodriguez, R., Lopez-Gonzalez, M.A. and Alva-Lopez, L.F. 2021. Diagnostic and neurological overview of brain tuberculomas: a review of literature. Cureus 13(12), 1–9. Rangel Guerra, R.A., Martinez, H.R., Garza, J.A. and Ancer, J. 1991. Brain-stem tuberculoma. Arch. Neurol. 48(4), 358–359. Schaller, M.A., Wicke, F., Foerch, C. and Weidauer, S. 2019. Central nervous system tuberculosis: etiology, clinical manifestations and neuroradiological features. Clin. Neuroradiol. 29(1), 3–18. Seputra, D.M.C.S., Suhendro, A.P., Sumada, I.K. and Yuliani, D. 2023. Intracranial tuberculoma in a patient with human immunodeficiency virus infection: a case report. Int. J. Adv. Med. 10(3), 254–257. Thakur, K., Das, M., Dooley, K.E. and Gupta, A. 2018. Global neurological burden of tuberculosis. Semin. Neurol. 38(2), 226–237. World Health Organization. 2023. Global tuberclosis report [Internet]. Geneva, Switzerland: World Health Organization. Available via https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023/tb-disease-burden | ||
| How to Cite this Article |
| Pubmed Style Firdawoke SN, Dibaba AD, Begna AK, Gebrewahd SH, Gizaw S. Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. J Microbiol Infect Dis. 2025; 15(1): 32-35. doi:10.5455/JMID.2025.v15.i1.4 Web Style Firdawoke SN, Dibaba AD, Begna AK, Gebrewahd SH, Gizaw S. Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. https://www.jmidonline.org/?mno=232447 [Access: April 26, 2025]. doi:10.5455/JMID.2025.v15.i1.4 AMA (American Medical Association) Style Firdawoke SN, Dibaba AD, Begna AK, Gebrewahd SH, Gizaw S. Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. J Microbiol Infect Dis. 2025; 15(1): 32-35. doi:10.5455/JMID.2025.v15.i1.4 Vancouver/ICMJE Style Firdawoke SN, Dibaba AD, Begna AK, Gebrewahd SH, Gizaw S. Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. J Microbiol Infect Dis. (2025), [cited April 26, 2025]; 15(1): 32-35. doi:10.5455/JMID.2025.v15.i1.4 Harvard Style Firdawoke, S. N., Dibaba, . A. D., Begna, . A. K., Gebrewahd, . S. H. & Gizaw, . S. (2025) Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. J Microbiol Infect Dis, 15 (1), 32-35. doi:10.5455/JMID.2025.v15.i1.4 Turabian Style Firdawoke, Surafel Nadew, Abdi Dandena Dibaba, Abera Kuma Begna, Selam Hagos Gebrewahd, and Samrawit Gizaw. 2025. Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. Journal of Microbiology and Infectious Diseases, 15 (1), 32-35. doi:10.5455/JMID.2025.v15.i1.4 Chicago Style Firdawoke, Surafel Nadew, Abdi Dandena Dibaba, Abera Kuma Begna, Selam Hagos Gebrewahd, and Samrawit Gizaw. "Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge." Journal of Microbiology and Infectious Diseases 15 (2025), 32-35. doi:10.5455/JMID.2025.v15.i1.4 MLA (The Modern Language Association) Style Firdawoke, Surafel Nadew, Abdi Dandena Dibaba, Abera Kuma Begna, Selam Hagos Gebrewahd, and Samrawit Gizaw. "Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge." Journal of Microbiology and Infectious Diseases 15.1 (2025), 32-35. Print. doi:10.5455/JMID.2025.v15.i1.4 APA (American Psychological Association) Style Firdawoke, S. N., Dibaba, . A. D., Begna, . A. K., Gebrewahd, . S. H. & Gizaw, . S. (2025) Unsuspected central nervous system tuberculosis presenting with dysphagia as a primary complaint: A diagnostic challenge. Journal of Microbiology and Infectious Diseases, 15 (1), 32-35. doi:10.5455/JMID.2025.v15.i1.4 |